Endoscopic Cyclophotocoagulation
| Primary authors |
|
|---|
The surgical management of glaucoma has evolved in recent years to go beyond procedures that make a hole in the eye to bypass the trabecular mesh-work to small-incision microsurgical techniques. These trends are similar to trends we have seen in cataract surgery, as well as in general surgery that are distinguished by smaller incisions, shorter procedure times, fewer complications, and faster recovery. In the cataract surgery realm, this can be seen with the ever-decreasing incision sizes for microincisional phacoemulsification and the development that follows with more sophisticated injectors and more flexible foldable lenses. In the general surgical realm, this evolution has been best demonstrated by the ubiquitous utilization of endoscopy, laparoscopy, or arthroscopy, technologies that afford the surgeon direct intraoperative visualization of focal pathology with incisions that are a mere fraction of the size compared with the large open incisions of the past. Endoscopic cyclophotoco-agulation (ECP) builds on this idea by having one of the smallest endoscopes manufactured to visualize the ciliary processes within the eye and treat the end organ with minimal, if any, collateral damage.
This chapter will review the physical aspects of the endoscopic cyclo-photocoagulator, the rationale for surgery using the device, the surgical technique, and my method for performing ECP. Also reviewed will be indications for surgery, preoperative and postoperative issues, and postoperative management, as well as special situations in which the endoscope can be utilized.
The Endoscopic Cyclophotocoagulation Device and Historical Perspective
The machine used to perform ECP is manufactured by Endo Optiks Inc (Little Silver, New Jersey). It is a microprobe diode laser endoscopy system that combines illumination, a video imager, and laser in a single handpiece. The endolaser probe has a 20- gauge diameter and can be used at the limbus or through pars plana to treat most types of glaucoma. Most frequently, it is used in combination with phacoemulsification. Transscleral cyclophotocoagulation (TCP) has been performed for many years using a variety of techniques, currently the most common being the Nd:YAG or diode lasers. Conventionally, these treatments have been used as a last resort for eyes that have failed multiple glaucoma surgeries, including trabeculectomy, and perhaps multiple glaucoma drainage devices. They also have been used to treat blind, painful eyes or eyes that have poor visual potential. TCP procedures are nearly impossible to titrate, and it is unclear what the intraocular pressure (IOP)-lowering results will be. They are also blind procedures, because the end organ that you wish to treat is not visualized and the procedures can be associated with high instances of hypotony, visual loss, pain, and inflammation.
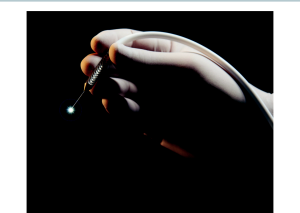
Alternatively, ECP does not cause collateral tissue damage because it targets the end organ tissue and treats the ciliary body alone. The endoscope itself has a tripartite construction and includes an image fiber, a light fiber, and a laser fiber that joins in a 20-gauge endoprobe, which is attached with a fiber optic cord to a console (Figures 15-1 and 15 -2). The laser provides a 110-degree field of view and depth of focus from 1 mm to 30 mm. The console contains a plug-in for each element of the laser probe, including the video camera, light source, video monitor, and a video recorder. The laser itself is a semiconductor diode tuned to 810 nm in wave length. The console allows you to adjust the strength of the laser power, the brightness of the light, and the brightness of the aiming beam, as well as the focus and orientation of the image. It also allows the laser to have a continuous burn versus an intermittent burn depending on the preference of the surgeon.
Indications for Endoscopic Cyclophotocoagulation
Endoscopic Cyclophotocoagulation Combined With Cataract Surgery
The vast majority of patients undergoing ECP are patients who have a cataract with concomitant glaucoma, and the ECP is performed at the time of cataract surgery. There is no fixed algorithm for choosing to do ECP in a patient with a cataract. One must consider that cataract surgery alone will likely lower the eye pressure several points; however, the longevity of this effect is uncertain. If the patient is on 1 to 3 glaucoma medications and is well controlled on medications, but wishes to have a lower medication burden
or is intolerant to medications these patients may get ECP in combination with cataract surgery to be on fewer medications. Another subgroup is those patients who have marginally controlled IOP on medications, and the surgeon and patient wish to get the IOP closer to the target pressure without changing any medications.
As a glaucoma specialist, I especially find ECP useful in patients who have had previous glaucoma surgery—either trabeculectomy, an Ex-Press shunt, or a conventional tube shunt—but need additional pressure lowering and happen to also have a visually significant cataract.
Plateau Iris Syndrome
Plateau iris syndrome poses an interesting situation in which the peripheral angle is narrow due to anterior rotation of the ciliary body. In plateau iris syndrome, even after peripheral iridotomy, the pressure may remain elevated because the mechanism of angle closure is not pupillary block but narrow peripheral angle due to anterior rotation of the ciliary processes.
In plateau iris, ECP combined with cataract surgery can be a very useful technique to definitively improve the angle of rotation of the ciliary body. During ECP, the shrinking of the ciliary processes rotates the ciliary body posteriorly. This technique has been referred to as endocylcoplasty.[1]
Pseudophakic and Aphakic Glaucoma
Patients who have had previous cataract surgery and have an in-the-bag intraocular lens (IOL) can undergo ECP. Although, the long-term results are less satisfactory than when ECP is combined with cataract surgery, this can be a useful technique in patients with scarred conjunctiva due to chemical injuries or in patients who have had multiple glaucoma surgeries in nearly every quadrant.
In aphakic glaucoma, ECP can be successfully performed; however, extra steps must be taken to prevent the eye from deflating during surgery, and typically an infusion port is required. ECP in an aphakic eye is typically not going to be a first option and typically would be performed after some form of glaucoma drainage implant has been unsuccessful and the eye has good vision. Therefore, it is desirable in those cases to avoid transscleral cyclophotocoagulation and the risk of decreased vision after the procedure.
The Phakic Eye
Endoscopic cyclophotocoagulation in a phakic eye has been described; however, it is my opinion that ECP in a phakic eye is rarely if ever appropriate, especially in an eye with good visual potential because of the degree of inflammation that will likely occur in a phakic eye and the risk of causing trauma to the lens with the instrumentation. In almost every case in which an eye is phakic with elevated IOP, it is better to consider other options besides ECP. ECP in a phakic eye is most likely going to create a cataract and cause adhesions between the lens capsule and the iris.
ECP vs TCP Combined with Cataract Extraction
Rodrigues and colleagues reported on the medium-term outcomes of combined phacoemulsification with TCP (phaco-TCP) versus phacoemulsification ECP (phaco-ECP) in patients with poorly controlled glaucoma and co-existing cataract.[2] This was a retrospective case series of 80 consecutive patients (46 eyes underwent phaco-ECP and 34 phaco-TCP) with at least 12-months follow-up. Success was defined as IOP between 6-21mmHg with ≥20% reduction and no further need for additional medication or surgery. The mean follow-up was 32.6 ±10.3 months. Success rate was greater with phaco-TCP than phaco-ECP (67.6% and 47.8%, P=0.037) and IOP was significantly lower after phaco-TCP (14.88 ±5.57mmHg, from 22.62±6.52) compared to phaco-ECP (18.07±6.72mmHg, from 22.83±7.88, P=0.0273). Topical glaucoma medication use was reduced similarly after phaco-TCP (from 3.38±0.88 to 2.65±1.04 medications, P=0.0012) and phaco-ECP (from 3.07±0.929 to 2.63±1.42 medications, P=0.0108). There were no cases of hypotony or decline in vision related to glaucoma or either surgical intervention and a similar number of patients required additional glaucoma surgery (phaco-ECP 15.2%, phako-TCP 5.9%, P=0.2884). The authors concluded that Phaco-TCP was more successful in controlling IOP than phaco-ECP with similar safety.
Technique
The usual technique for cataract surgery combined with ECP starts out essentially the same way as any typical cataract surgery using phaco-emulsification. The only exception is I typically make a second incision 180 degrees from my original temporal keratome incision to facilitate a full 360 degrees of treatment. If you are using a curved endoprobe, 270 degrees of ECP can be performed through 1 wound; however, the pressure-lowering effects will not be as significant as 360 degrees of treatment.[3] The ECP probe will fit through the small incision keratome wounds that are currently being used for phacoemulsification. I typically make a 1.8-mm keratome incision; however, the probe will fit through a port as small as 1.5 mm and still allow the flexibility and maneuverability required.
After successful phacoemulsification and implantation of the IOL, it is important to fully remove the viscoelastic from the capsular bag. Visco-elastic is then injected into the sulcus. I typically use Healon GV because it provides superior visualization of the entire ciliary body and also the best view of the posterior ciliary processes. This superior view is created because the Healon not only lifts the iris but it also pushes down the anterior capsule and gives space to aim the laser through the zonules toward the posterior processes to get a maximum IOP-lowering effect.
It should be noted that ECP can be performed before implanting the IOL, but great care must be taken not to rupture the capsular bag. The advantage of doing ECP prior to implanting the lens is that it allows the surgeon to laser through the bag and get the very posterior aspects of the ciliary body; however, I rarely perform this technique because I have found that the Healon GV allows for excellent visualization of this area with the IOL in place.
Combined Endoscopic Cyclophotocoagulation and Cataract Surgery
I prefer to first treat the area of the ciliary processes that are 180 degrees from the temporal wound, treating from left to right with a curved probe. Once the aiming beam is over the center of the ciliary process, the foot pedal is depressed and the laser is used to “paint” the ciliary processes in one smooth motion from left to right, treating not only the center but also the valleys in between. Great care is given to avoid treating the iris itself and also from overtreating the processes causing a “pop.” Avoiding this overtreatment minimizes postoperative inflammation, making the procedure similar or slightly more inflammatory than what is seen with standard cataract surgery.
After the first 180 to 270 degrees are treated, I then take the viscoelastic and viscodilate the subincisional temporal sulcus and repeat the steps above to get a full 360-degree treatment. Once this has been completed, the probe is slowly removed from the eye, taking care to visualize its path as it exits the eye. The viscoelastic must then be carefully removed. If it is not fully removed there will be a high likelihood of a postoperative IOP spike. Because of the risk of postoperative IOP spikes, it may be appropriate to use either a direct- or indirect-acting injection of a miotic agent in the anterior chamber to improve postoperative aqueous outflow.
Endoscopic Cyclophotocoagulation in Pseudophakes and Aphakes
If the patient is pseudophakic undergoing ECP, the technique is essentially identical to when it is combined with cataract surgery. If the patient has an anterior chamber IOL, ECP is not going to be possible, and likely if there is an iris-fixated or scleral-fixated IOL, ECP will also be contraindicated because of the risk of disrupting the iris sutures. However, in most cases of pseudophakia, one can viscodilate the sulcus and the viscoelastic can often break any adhesions that might be found.
Aphakic glaucoma poses an entirely different problem because often aphakic eyes are unicameral, and when you enter the eye, it will deflate. Typically, an anterior chamber maintainer is required. I use a Lewicky (Beaver-Visitec, Waltham, Massachusetts), which is attached to the phaco-emulsification machine and is inserted through a paracentesis placed in a different quadrant from the wound. Usually viscoelastic is unnecessary in an aphakic eye unless a remnant of the capsular bag is opacified. The anterior chamber maintainer serves to constantly irrigate balanced salt solution into the eye to provide chamber stability and an adequate view. If any anterior vitreous is visible, this must be removed by vitrectomy prior to the ECP.
It is possible that due to visibility issues in an aphakic patient, an anterior incision may be impossible and the pars plana approach may be needed. Moreover, the pars plana approach may also be preferred in eyes with anterior chamber IOLs. In the presence of a crystalline lens, ECP is contraindicated for both the anterior and pars plana approach. During the pars plana approach, you also must be certain that vitreous is not present and the laser endoscope is inserted through the pars plana at 3.5 to 4 mm posterior to the limbus.
Pediatric Glaucoma
Endoscopic cyclophotocoagulation can be performed in the pediatric patient population.[4] However, unlike the adult population, ECP in the pediatric patient is typically reserved for refractory glaucoma in which the patient is already aphakic or pseudophakic and has had the maximum amount of the usual anterior segment glaucoma surgery (ie, goniotomy, trabeculotomy, 360-degree trabeculotomy, and/or 1 or 2 tube shunts).
ECP may be used in a child’s eye with good visual potential after multiple glaucoma surgeries, especially in eyes with pediatric glaucoma secondary to congenital cataracts. I have not attempted ECP in eyes with primary congenital glaucoma; however, one could argue that after these children reach adulthood and develop cataracts, cataract surgery combined with ECP may be an option for them.
Other Refractory Glaucoma
ECP has also been described for the treatment of refractory glaucomas;[5] however, ECP should be avoided in patients with uveitic glaucoma because ECP will likely worsen the inflammation.
Postoperative Considerations
Postoperative medications after ECP mirror those which are used for cataract surgery alone. These include a nonsteroidal anti-inflammatory drop, as well as a fourth-generation fluoroquinolone. With the advent of Durezol (difluprednate) I have found that treatment with this medication 4 to 6 times daily has greatly reduced postoperative inflammation with ECP. I typically taper the Durezol over a 4- to 6-week period; however, care must be taken to avoid a steroid response. Moreover, due to the more dispersive action of the viscoelastic used during ECP and the high risk for IOP spikes, I typically will give patients acetazolamide after the procedure.
Typically, at the first postoperative visit, if the patient is on 1 to 3 glaucoma medicines, I will stop 1 medication, and continuing the other medications, depending on the IOP that day. Then I have the patients follow up in 5 to 7 days and titrate the medications depending on the IOP.
Conclusion
Endoscopic cyclophotocoagulation is an effective treatment for lowering IOP, but it has been surrounded by some controversy. I do not perform ECP on every patient in my practice with a cataract and concomitant glaucoma who is on medications. Cataract surgery combined with ECP in patients who are poor candidates for glaucoma filtration surgery or who had a poor experience with glaucoma filtration surgery in 1 eye and need a procedure in their other eye, can be extremely satisfying for both the patient and the surgeon. ECP is also a helpful option in monocular patients or patients who have a bleeding diathesis due to anticoagulants, whereas in the later situation, hyphema can often occur with glaucoma filtration surgery.
A major benefit of ECP is that it avoids the complications that are associated with transscleral cyclophotocoagulation, namely hypotony, severe inflammation, and phthisis. Due to the fact that only the anterior third of the ciliary processes are treated with ECP, hypotony is an extreme rarity.
It should be noted that patients with advanced glaucoma and con-comitant cataract who are on multiple glaucoma medications most often require combined phacoemulsification with the Ex-Press mini glaucoma device or phacotrabeculectomy. I typically perform cataract surgery combined with the Ex-Press mini glaucoma shunt in these cases.[6] Phaco combined with ECP is typically reserved for patients with mild glaucoma, as indicated above. However, as previously mentioned, monocular eyes can be considered for ECP in advanced glaucoma; however, the patient must be counseled that they may need some sort of filtration surgery or a nonpenetrating surgery, such as canaloplasty, because the effects of the combined cataract surgery and ECP may not be adequate to keep the patient at target IOP.
The endoscopic laser can also be used for a variety of other things such as anterior chamber visualization to perform synechialysis. Therefore, rather than doing goniosynechialysis, one can perform endosynechialysis. The endolaser is also very helpful in cases of traumatic glaucoma in which there might be issues with visibility. Recently, using the endolaser to close a cyclodialysis cleft has been described. [7]
In this modern age of glaucoma surgery in which there are multiple innovations to improve patient results and lower complication rates, it is helpful to have a broad palette of options to cater the treatment of glaucoma to the individual patient. Endoscopic cyclophotocoagulation is one more vivid color on the surgical palette for the treatment of glaucoma.
Key Points
- ECP is primarily used in conjunction with cataract surgery to lower IOP in patients with glaucoma.
- ECP is safe and effective if performed in the proper manner and only causes minimal inflammation if the surgeon does not “over-treat.”
- ECP can be especially useful in patients with plateau iris syndrome, aphakic glaucoma if an infusion port is used, and in other refractory glaucomas after more conventional glaucoma surgery has been performed.
- The endoscope can be used for visualization of the angle during syn-echialysis, during cyclodialysis repair, or perhaps to assist with visualization during minimally invasive glaucoma surgery (MIGS) such as trabecular bypass into Schlemm’s canal or the suprachoroidal space, in lieu of a goniolens.
References
- ↑ Podbielski DW, Devesh K. Varma DK, Tam DY, Ahmed IK. Endocycloplasty. A new technique for managing angle-closure glaucoma secondary to plateau iris syndrome. Glaucoma Today. October 2010.
- ↑ Rodrigues IA, Bloch E, Lim WS, Saurabh G. Phacoemulsification Combined with Endoscopic Versus Transscleral Cyclophotocoagulation in Poorly Controlled Glaucoma - A Comparative Case Series. Journal of Glaucoma: November 05, 2019 - Epub Ahead of Print.
- ↑ Kahook MY, Lathrop KL, Noecker RJ. One-site versus two-site endoscopic cyclophoto-coagulation. J Glaucoma. 2007;16(6):527-530.
- ↑ Carter BC, Plager DA, Neely DE, Sprunger DT, et al. Endoscopic diode laser cyclopho-tocoagulation in the management of aphakic and pseudophakic glaucoma in children. JAAPOS. 2007;11(1):34-40.
- ↑ Lin SC. Endoscopic and transcleral cyclophotocoagulation for the treatment of refractory glaucoma. J Glaucoma. 2008;17(3):238-247.
- ↑ Kanner E, Netland PA, Sarkisian SR, Du H. Ex-Press miniature glaucoma device implanted under a scleral flap alone or combined with phacoemulsification cataract surgery. J Glaucoma. 2009;18(6)488-491.
- ↑ Caronia RM, Sturm RT, Marmor MA, Berke SJ. Treatment of a cyclodialysis cleft by means of ophthalmic laser microendoscope endophtocoagulation. Am J Ophthalmol. 1999;128(6):760-761.