Intraocular Pressure Lowering Medications
| Primary authors |
|
|---|
Lectures on Medical Management of Glaucoma:
- Medical Treatment of Glaucoma (Part I with Cara Capitena Young, MD) https://youtu.be/ma1FNm7daMQ
- Medical Treatment of Glaucoma (Part II with Cara Capitena Young, MD) https://youtu.be/Hd40_4FEIsg
- Medical Treatment of Glaucoma (Part III with Cara Capitena Young, MD) https://youtu.be/q2Gu83oYqPQ
- Adherence to Glaucoma Therapy (Part I) https://youtu.be/xTaZfL4s0BM
- Adherence to Glaucoma Therapy (Part II) https://youtu.be/cR4ymlxy2jg
- Glaucoma Therapy in the Setting of Pregnancy and Breastfeeding (Malik Y. Kahook, MD) https://www.youtube.com/watch?v=tY0NXOKU7aU
- Rhopressa, Rocklatan and Vyzulta (Malik Y. Kahook, MD) https://www.youtube.com/watch?v=dQGTSHiUcvA
- Reticular Bullous Epithelial Edema With ROCK Inhibitor Therapy (Malik Y. Kahook, MD) https://www.youtube.com/watch?v=otWWsyJzE9g&t=1s
- Should I prescribe oral statin therapy for my glaucoma patients? (Malik Y. Kahook MD) https://www.youtube.com/watch?v=y0fVhzypvyo
MEDICAL MANAGEMENT OF GLAUCOMA
Deitz GA, Capitena Young C, SooHoo JR, Ertel MK, Seibold LK, Kahook MY
Glaucoma is an optic neuropathy associated with progressive loss of retinal ganglion cells (RGCs), optic nerve atrophy, and characteristic patterns of visual field loss. Elevated intraocular pressure (IOP) is the predominant modifiable risk factor of onset and progression of the disease. In many patients diagnosed with ocular hypertension and/or glaucoma, topical medication to lower IOP is often employed as first line treatment. Several landmark trials (Collaborative Normal Tension Glaucoma Study, Ocular Hypertension Treatment Study, United Kingdom Glaucoma Treatment Study) have demonstrated that medically lowering IOP reduces the risk of glaucoma development and disease progression (Kass et al, 2002; Garway-Heath et al, 2013; Danias et al, 1999).
Modern medical therapies to treat glaucoma target aqueous humor dynamics through a variety of biochemical pathways, ultimately either reducing formation or increasing outflow of aqueous humor, to reduce IOP. However, not all IOP-lowering medications are equal. Individual patient characteristics and comorbidities should always be taken into consideration prior to starting any medical therapy. Topical glaucoma medications, despite being a localized therapy, can have systemic adverse effects due to absorption through the nasolacrimal system and lack of first-pass hepatic metabolism. This potential for systemic absorption must be accounted for in every patient, however, can be minimized with the use of punctal occlusion.
Below is a brief review of the different classes of IOP-lowering medications, their mechanism of action, side effect profiles and adverse effects, as well as several important considerations for patient selection.
OUTLINE
o When to use IOP lowering medications
o Limitations to IOP lowering medications
o Medication classes
o Beta-blockers
o Alpha-agonists
o Prostaglandin analogs
o Carbonic anhydrase inhibitors
o Parasympathomimetic/miotic agents
o Rho kinase inhibitors
o Hyperosmotics
o Fixed combinations
o Treatment approach
o Age
o Pregnancy (pre- and post-partum)
o Adherence difficulty
o Comorbidities
o Unilateral disease
o Ocular surface disease and Benzalkonium Chloride (BAK) sensitivity
WHEN TO USE IOP LOWERING MEDICATIONS
While every patient requires an individualized treatment approach, IOP-lowering medications are often the most appropriate first line treatment in several scenarios. Specifically, medication can act as a bridge to more permanent treatment such as laser or incisional surgery in cases of congenital glaucoma, angle-closure glaucoma, and some forms of secondary glaucoma. Additionally, topical therapy is often used in patients who are at high risk of surgical or laser-related complications, as well as those hesitant to proceed with these more invasive treatment options. Notably, the proportion of patients who are reluctant to undergo invasive glaucoma treatment is likely not insignificant. In one small study, the number of patients who preferred to continue using topical IOP lowering medications rather than escalate care was 55% (SooHoo et al, 2016). In patients with primary open angle glaucoma or ocular hypertension, IOP-lowering medication can be used as the first-line therapy and, in cases of adequate response and good tolerance, can be the only treatment modality in the management of their disease.
LIMITATIONS TO IOP LOWERING MEDICATIONS
There are several major limitations to the use of IOP lowering medications in clinical practice, such as lack of efficacy and intolerable adverse effects, however, the most important limitation is patient compliance. Depending on the study and definition of noncompliance, the proportion of patients who deviate from their prescribed IOP-lowering medication regimen ranges from 5% to 80% (Olthoff et al, 2005). Knowledge about glaucoma, specifically the disease course and consequences, has been shown to be positively associated with medication compliance (Mansouri et al, 2011). However, because of the slowly progressive nature of glaucoma, it can be difficult for patients to appreciate the necessity of treatment as they are often not symptomatic from their disease. Factors which are inversely associated with medication compliance include number and frequency of dosing (Robin et al, 2005; Olthoff et al, 2005), difficulty with drop administration, forgetfulness, difficulty reading instructions, financial burden, as well as adverse effects (Lacey et al, 2008; Stryker et al, 2010; Friedman et al, 2008).
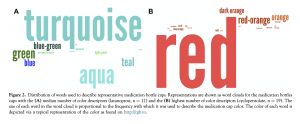
Unlike pills administered orally which are often of varying sizes, shapes, and colors, the distinction between different topical glaucoma medications can be a source of confusion for patients given the similar appearance of ophthalmic bottles. Different classes of glaucoma medications are administered at different frequencies and times of day, and inappropriate use can alter the IOP lowering effect and increase the likelihood of experiencing adverse effects. The ophthalmic bottle cap color is the most commonly used method by which patients differentiate ophthalmic medications, followed by the bottle size/shaped, and name on the bottle. In fact, in one study, only 18.5% of patients used the medication name to distinguish between different topical glaucoma medications (Marando et al, 2015). However, not even identification by cap color is flawless. In patients with more severe glaucoma (and resultant acquired color vision deficiency), and in situations where patients and providers use a high heterogeneity of color descriptors to communicate (Figure 1), there is significant disagreement regarding medication identification based on cap color (Dave et al, 2015).
These are important considerations for providers to keep in mind when treating patients with IOP lowering medications. While administration of ophthalmic medications is routine in most ophthalmology clinics, it should never be assumed that patients will be able to similarly administer these mediations correctly at home. Difficulty with medication compliance should always be considered when faced with a decision to escalate treatment in the setting of inadequate response.
MEDICATION CLASSES
Beta blockers (-Blockers): Levobunolol, carteolol, metipranolol, timolol maleate, timolol hemihydrate, betaxolol
Mechanism of Action:
Beta-1 (-1) and beta-2 (-2) receptors are expressed throughout the eye. An increase in aqueous humor formation is triggered by a rise in cyclic adenosine monophosphate (cAMP) in the non-pigmented ciliary epithelial cells of the ciliary processes (Neufeld et al, 1972; Bartels et al, 1987). This process is mediated by beta agonist activity. The antagonism of these receptors reduces intracellular cAMP production, leading to a reduction in aqueous humor production. Medications which bind to both classes of beta receptors (-1 and -2) are termed nonselective, whereas those that only bind to one type are called selective. All of the above listed medications are non-selective except betaxolol, which is the only β-1 selective antagonist. Because of its selective nature, it is less likely to cause pulmonary side effects compared to non-selective beta blockers, due to the presence of β-2 receptors on bronchial smooth muscle cells (Ofner et al, 1987).
Efficacy:
Beta blockers have been shown to reduce IOP, on average 20-30% from baseline (Stewart, 1986; van der Valk et al 2005). A study comparing the efficacy of timolol, betaxolol, and carteolol found no significant difference in IOP lowering effect at 12 months, though efficacy did begin to differ between the three medications over the following five-year follow-up period, albeit not significantly (Watson et al, 2001). Timolol’s effect on aqueous humor production occurs within one hour of instillation with a peak reduction after two hours and measurable effect for up to 24 hours (Ramakrishan et al, 2013). Notably, as a class, beta blockers are less effective at lowering nighttime IOP compared to other topical medication classes, as aqueous production is already down regulated at night (Orzalesi et al, 2000).
Adverse Effects:
Overall, beta blockers are one of the most well tolerated topical IOP-lowering medications. The adverse effects patients do experience with these medications can be understood given the ubiquity of beta receptors throughout multiple organ systems. Antagonism of -1 receptors found on cardiac myocytes lead to reduction in chronotropy and inotropy, and antagonism of -2 receptors on bronchial smooth muscle lead to contraction and increased airway resistance (Taylor, 2007).
o Local adverse effects include burning and stinging upon instillation, blepharoconjunctivitis, alopecia, and contact dermatitis.
o Systemic effects include those affecting the cardiovascular (CV) system such as bradycardia, arrhythmia, syncope, hypotension, reduced exercise tolerance; the pulmonary system (bronchoconstriction and exacerbation of obstructive lung disease); neuropsychiatric (lethargy, mood changes, depression, CNS depression; serum lipid levels (increase triglycerides and low-density lipoprotein cholesterol, decrease high-density lipoprotein cholesterol) though the clinical impact of this is likely not significant; impotence and reduced libido; masking of the effects of hypoglycemia; and exacerbation of myasthenia gravis.
o Because of the potential for CV adverse effects, it is prudent to measure pulse prior to initiating therapy with topical beta blockers due to the potential for heart block and/or bradycardia.
Other Considerations:
o Beta blockers are often dosed twice daily, though they can just as effectively be dosed once daily in some patients (those with bothersome local or systemic side effects) given the lack of significant between-group differences in IOP in patients treated with 0.25% timolol ophthalmic solution once daily or twice daily (Soll, 1980). If using beta blockers once daily, it is prudent to time use with natural variations in blood pressure (BP), and not administer in the evening when BP is often at its lowest, or at the same time as administration of a short acting BP medication.
o Patients already on a systemic beta blocker may not respond to topical beta blockers with a significantly lower IOP (Khawaja et al, 2014).
o Timolol 0.25% and timolol 0.5% have similar efficacy and safety profiles (DuBiner et al, 1996).
o Beta blockers are known to be associated with a dissipation phenomenon referred to clinically as short-term “escape” and long-term “drift”, which describes the reduction of efficacy of medication over the time period of days to weeks, or over the course of years, respectively (Boger, 1983). This phenomenon is representative of tachyphylaxis, a term referring to the decrease in response to a drug after it’s administration (Webb et al, 2011).
o Short-term “escape” is likely the result of receptor saturation and subsequent up-regulation of beta receptors, leading to a reduction in medication efficacy. Long-term drift is likely the result of prolonged medication use, and subsequent reduction in response to agonist in the setting of constant exposure (Boger, 1983).
o Avoid using beta blockers in patients on strong CYP450 inhibitors, as they can increase the plasma concentration and increase risk of CV side effects (Shin et al, 2009).
o Use beta blockers with caution in children due to the potentially high systemic levels achieved (Freedman et al, 2006).
o Carteolol, a non-selective beta blocker, does have some intrinsic sympathomimetic activity which limits its CV and pulmonary side effects (Frishman et al, 1990).
o Timolol is available in a BAK-free formulation.
Alpha Agonists (⍺-Agonists): Epinephrine, dipivefrin, apraclonidine, brimonidine tartrate
Mechanism of Action:
The eye contains both ⍺-1 and ⍺-2 adrenergic receptors. These are G-protein coupled receptors which, when activated, lead to a reduction of adenylate cyclase and intracellular cAMP. Stimulation of ⍺-1 receptors result in contraction of the iris dilator and Muller muscles (leading to mydriasis and lid retraction), as well as vasoconstriction resulting in restricted blood flow to the ciliary muscle (leading to reduced production of aqueous humor) (Docherty, 2009). Stimulation of ⍺-2 receptors similarly result in ciliary body vasoconstriction as well as episcleral vasoconstriction (Reitsamer et al, 2006). ⍺-2 receptors are also found in retinal ganglion cells, and when stimulated by ⍺-2 agonists, have been shown to significantly reduce retinal ganglion cell loss in the setting of optic nerve crush injury in experimental and animal models (Wheeler et al, 2001). The first alpha agonists to be used for IOP reduction were nonselective (epinephrine, dipivefrin), however these are infrequently used today with the advent of selective ⍺-2 agonists such as brimonidine and apraclonidine (Arthur et al, 2011).
Efficacy:
Brimonidine has been proven to reduce baseline IOP by approximately 17% according to a meta-analysis of published clinical trials (van der Valk et al 2005), and apraclonidine by between 20-23% (Schadlu et al 1998). The peak effect of brimonidine is achieved 1-2 hours after use (Walters, 1996), whereas the peak effect of apraclonidine is achieved more rapidly. It is for this reason that apraclonidine is commonly used perioperatively to prevent IOP spikes after laser and surgical procedures but avoided for long-term use due to the high incidence of blepharoconjunctivitis and tachyphylaxis (Pollack et al, 1988).
Adverse Effects:
o Local adverse effects include burning and stinging upon instillation, blepharitis, blepharoconjunctivitis, hyperemia, blurry vision, follicular conjunctivitis, aggravation of ocular surface disease, and granulomatous anterior uveitis. Local adverse effects of non-selective agonists, specifically, include eyelid retraction and mydriasis.
o Systemic effects include bradycardia, systemic hypotension, orthostatic hypotension, rhinitis, xerostomia, facial edema, taste perversion, and neuropsychiatric (especially when used along with medications which are Central Nervous System (CNS) depressants).
Other Considerations:
o Alpha agonists are contraindicated in infants or young children due to risk of CNS depression, apnea, bradycardia, hypotension (Arthur et al, 2011).
o Alpha agonists as a medication class have a relatively high incidence of local intolerance.
o Alpha agonists are contraindicated for use in patients on certain antidepressants due to the risk of precipitation of hypertensive crisis with concurrent use of monoamine oxidase inhibitors (MAOIs), and increased risk of CNS depression with concurrent use of tricyclic antidepressants (TCAs) (Schacknow et al, 2010).
Carbonic Anhydrase Inhibitors
Mechanism of Action:
Carbonic anhydrase enzymes represent a family of intracellular enzymes which catalyze the reversible interconversion between carbon dioxide and water, and the positively charged hydrogen ion and negatively charged bicarbonate ion (Sly et al, 1995). In the eye, carbonic anhydrase enzymes in the nonpigmented epithelium generate hydrogen and bicarbonate ions, allowing water to enter the cells, leading to aqueous humor production (Delamere, 2005). Carbonic anhydrase inhibitors are sulfonamide compounds which act directly on this enzyme to inhibit the production of aqueous humor. Approximately 99% of the enzymatic activity needs to be inhibited to result in a measurable reduction in aqueous humor production (Maren et al, 1967). As a class, carbonic anhydrase inhibitors can be utilized for their diuretic effect due to the activity of carbonic anhydrase in the proximal convoluted tubule of the kidney. Inhibition of the enzyme in this organ system causes increased urinary loss of bicarbonate ions leading to a mild diuretic effect as well as a metabolic acidosis (Aronson et al, 2011).
Carbonic anhydrase inhibitors, topical: Dorzolamide hydrochloride, brinzolamide
Efficacy:
Of the two topical carbonic anhydrase inhibitors currently available, brinzolamide has demonstrated efficacy of 17% reduction in IOP from baseline compared to a 22% reduction of IOP peak with dorzolamide (van der Valk et al, 2005). Notably, there is no benefit to adding a topical carbonic anhydrase inhibitor if a patient is already on an oral agent of this class (Rosenberg et al, 1998).
Adverse Effects:
o Local adverse effects include burning and stinging upon instillation, bitter after-taste often referred to as metallic, punctate keratopathy, corneal decompensation in eyes with pre-existing endothelial cell function, and blurred vision with brinzolamide due to formulation in suspension (Detry-Morel, 2006).
o Systemic effects are minimal, but include a possible loss of energy and taste disturbance (Detry-Morel, 2006)
Carbonic anhydrase inhibitors, systemic: Acetazolamide, methazolamide
Efficacy:
Oral acetazolamide reduces aqueous flow by 30%, compared to a 17% reduction with topical dorzolamide (Maus et al 1997). Systemic administration allows for more rapid time to action, with the peak effect of IV acetazolamide occurring within 15 minutes of administration. While systemic carbonic anhydrase inhibitors may be more effective than topical, the adverse effects limit their use in some patients. Up to 50% of people cannot tolerate these adverse effects (Kobayashi et al, 2000).
Adverse Effects:
As previously mentioned, carbonic anhydrase inhibitors are sulfonamide derivatives and though cross-reactivity is low, they may be associated with severe allergic reaction and even anaphylaxis. Other adverse effects include crystalluria, paresthesia, weight loss, loss of energy, taste disturbance especially with carbonated beverages, loss of libido and impotence, gastrointestinal (GI) upset, kidney stones, metabolic acidosis, electrolyte imbalance, depression, blurred vision. Rare but serious adverse effect include aplastic anemia, as well as leukopenia, pancytopenia, and agranulocytosis. (Detry-Morel, 2006)
Other Considerations:
o Typical dosing of oral carbonic anhydrase inhibitors: methazolamide 25-50mg BID or TID, acetazolamide 250mg QID or 500mg BID for sustained release tablets. The pediatric dose is 5-10mg/kg every 4-6 hours.
o Not only does methazolamide have a longer half-life than acetazolamide, it undergoes first-pass hepatic metabolism, which lessens the risk of adverse effects (Sambhara et al, 2013).
o Use acetazolamide with caution in patients with kidney disease. Depending on severity of kidney disease, these patients may need dose adjustment as it is renally excreted (Bartlett, 2013).
o Methazolamide is also less likely to cause acidosis and thus, renal lithiasis. Methazolamide is metabolized hepatically, so use is not recommended in patients with liver disease/cirrhosis (Bartlett, 2013).
o Avoid use of carbonic anhydrase inhibitors in patients with sickle cell trait or sickle cell disease due to increase in sickling of erythrocytes with use (Bartlett, 2013).
o Avoid use of carbonic anhydrase inhibitors in patients with hepatic cirrhosis, as urine alkalization causes increased serum ammonia levels and can lead to the development of hepatic encephalopathy (Bartlett, 2013).
o Dorzolamide is available as BAK-free formulation
Prostaglandin analogs: Latanoprost, bimatoprost, travoprost, tafluprost, unoprostone isopropyl, latanoprostene bunod
Mechanism of Action:
Prostaglandins are lipid compounds resulting from the metabolism of arachidonic acid. There are nine established prostaglandin receptors in the human body, differentiated by the prostaglandin to which they bind most specifically to (Winkler et al, 2014). Of these nine receptors, five have been identified in ocular tissue, including the trabecular meshwork and Schlemm’s canal cells. These five include: prostaglandin FP receptor (PGFP), as well as all four PGE receptors (EP1-4). Prostaglandin analogues are prodrugs of prostaglandin F2⍺ (PGF2⍺) that become biologically active via hydrolyzation by corneal esterase. These medications are thought to predominantly increase aqueous humor outflow via the unconventional pathway, though a growing understanding of their mechanism of action suggests a role in increasing outflow through the conventional pathway as well. (Schlotzer-Schrehardt et al, 2002)
o Unconventional pathway: PGF2⍺ and prostaglandin analogues bind to EP and FP receptors in the ciliary muscle, resulting in relaxation and increased aqueous humor outflow as well as disruption of remodeling of the extracellular matrix (Lütjen-Drecoll et al, 1988). PGF2⍺ and prostaglandin analogues appear to upregulate matrix metalloproteinases (MMPs), which degrade and remodel the extracellular matrix, while maintaining tissue inhibitor of metalloproteinase (TIMPs) expression, which inhibit MMPs expression. This ultimately increases remodeling and turnover of ciliary muscle extracellular matrix. (Gaton, 2001)
o Conventional pathway: Outflow of aqueous humor appears to be increased by prostaglandin analogs via focal loss of extracellular matrix in the juxtacanalicular region of the trabecular meshwork (through similar alteration of MMPs as previously mentioned), as well as cellular separation of the inner walls from the basal lamina of Schlemm’s canal (Bahler et al, 2008).
Efficacy:
Prostaglandin analogs are the most effective topical agent for reducing IOP (van der Valk et al, 2005) and for this reason, as well as the ease of once daily dosing, are often employed as the first-line agent in the treatment of open angle glaucoma. The majority of trials comparing bimatoprost, travoprost, and latanoprost have reported relatively equivalent degrees of IOP reduction (Parrish et al, 2003). The IOP reduction ranges from 28-29% from trough and 31-33% from peak time points (van der Valk et al, 2005). 24-hour studies have indicated that prostaglandin analogs (as well as fixed combinations discussed later) significantly reduce 24-hour fluctuation of IOP (Stewart et al, 2008).
Latanoprostene bunod (Vyzulta, Bausch Health) is a novel nitric-oxide donating prostaglandin analogue found to be slightly more efficacious than both timolol and latanoprost (Addis et al, 2018). Latanoprostene bunod is metabolized into an F2α prostaglandin analog, and butanediol mononitrate. The F2α prostaglandin analog acts in a mechanism described above, whereas the butanediol mononitrate component acts as a nitric oxide donor which leads to alterations in cytoskeleton proteins, resulting in relaxation of the trabecular meshwork and increase in aqueous humor outflow (further described below) (Cavet et al, 2018).
Adverse Effects:
o Local adverse effects include burning and stinging upon instillation, conjunctival hyperemia, hypertrichosis and hyperpigmentation of eyelashes (reversible with drug discontinuation), darkening of irides (a permanent effect), darkening of the eyelids (reversible), periorbital fat atrophy (may be reversible with drug discontinuation), macular edema development in patients after cataract extraction with intraocular lens (IOL) implantation (CE/IOL) with compromised posterior capsule (Detry-Morel, 2006), and potential to mediate herpes simplex virus (HSV) epithelial keratitis (Wand et al, 1999).
o Systemic effects include flu-like symptoms, muscle/joint pain, non-ocular eczema, and asthma exacerbation (Detry-Morel, 2006).
Other Considerations:
o Some patients may respond to one agent of PGA over another, so switching medication after a 4-6 weeks trial is reasonable before switching to an entirely different class.
o Latanoprost, travoprost, and tafluprost are available as BAK-free
o Latanoprost BAK-free microemulsion is marketed as being better for patients with ocular surface disease.
Parasympathomimetics (miotics): Pilocarpine, carbachol, echothiophate, demecarium
Mechanism of Action:
Parasympathomimetics or miotics work to lower IOP by stimulating the longitudinal ciliary muscle, causing loss of accommodation and creating traction on the scleral spur and trabecular meshwork, thereby opening the angle and facilitating aqueous humor outflow. They also act on the iris sphincter, causing miosis (Goel et al, 2010). The two classes of parasympathomimetics or miotics include direct-acting cholinergic agonists (acetylcholine, carbachol, pilocarpine) and indirect-acting anticholinesterase agents (ecothiophate, demecarium; which are no longer in use).
Efficacy:
Peak IOP lowering effect of pilocarpine occurs within two hours and lasts for at least eight hours. IOP reduction of 20% is seen 2-8 hours after dosing, and 14-15% thereafter (12-15 hours) (Drance et al, 1974).
Adverse Effects:
o Local adverse effects include pupillary constriction, ocular burning, brow ache, induced myopia, retinal detachment, reduced night vision, accommodative spasm, and increased permeability of blood/aqueous barrier leading to increased inflammation.
o Systemic adverse effects include diarrhea, abdominal cramps, increased salivation, bronchospasm, and enuresis.
Other Considerations:
o Adverse effects occur more frequently and with higher severity with carbachol use compared to pilocarpine.
o Depolarizing muscle relaxants (succinylcholine) cannot be used for up to 6 weeks after stopping indirect-acting agents (Shiroma et al, 2015).
o Adverse effects with ecothiophate are more severe (cataract formation, retinal detachment, iris cyst formation) compared to other parasympathomimetic IOP lowering medications.
o Four times a day dosing of pilocarpine can make it difficult for chronic use.
Rho kinase inhibitors: Ripasudil, netarsudil
Mechanism of Action:
Rho kinase inhibitors are a relatively new class of glaucoma medications, thought to lower IOP by modulation of the actomyosin cytoskeleton of cells of the trabecular meshwork and Schlemm’s canal, resulting in cellular relaxation and increase in aqueous humor outflow. Additionally, the Rho kinase inhibitors may increase optic nerve head vasodilation, increasing optic nerve perfusion (Tanna et al, 2018). Rho kinase inhibitors have also been shown to promote retinal ganglion cell survival and optic nerve axon regeneration after damage in animal models (Shaw et al, 2017). There are two isoforms of Rho kinase, both of which are serine/threonine kinases, called ROCK1 and ROCK2. Both ripasudil and netarsudil are ROCK1s, though netarsudil also has antagonistic activity against norepinephrine transport, preventing norepinephrine release from presynaptic nerve terminals, and leading to a decrease in production of aqueous humor in the same pathway as that acting on by ⍺-2 receptor agonists (Moshirfar et al, 2018).
Efficacy:
In phase II/III clinical trials, ripasudil lowered IOP by mean 3.7 mmHg, and netarsudil by mean 5.5 mmHg (Lu et al, 2017). Compared to latanoprost, netarsudil 0.01% and netarsudil 0.02% have a lower IOP reduction, though the reduction is dose dependent with netarsudil – 5.5 mmHg in 0.01% and 5.7 mmHg in 0.02% dosing (Mehran et al, 2020).
Adverse Effects:
o Local adverse effects include conjunctival and episcleral vascular dilation, conjunctival hyperemia, blepharitis, allergic conjunctivitis, instillation site pain, and corneal verticillata (not known to be visually significant) (Serle et al, 2018)
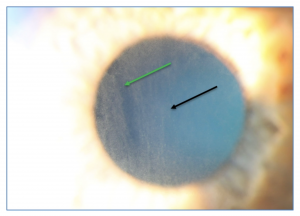
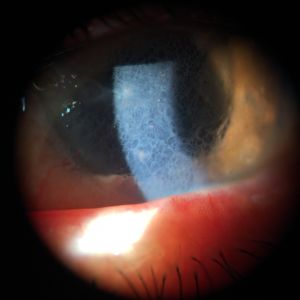
o Reticular Bullous Epithelial Edema With ROCK Inhibitor Therapy: https://www.youtube.com/watch?v=otWWsyJzE9g&t=1s
This clinical presentation appears to be related to initiation of a ROCK inhibitor in patients with pre-existing compromised corneal endothelial dysfunction (Fuch's, trauma, etc). The edema appears within days or weeks of starting therapy and typically resolves weeks after discontinuation. The specific pathophysiology of this process is still under investigation.
o Systemic adverse effects are typically minimal.
Other Considerations:
o Some studies have reported side effects to be transient and resolve spontaneously (Sakamoto et al, 2019).
Hyperosmotics: Glycerin (oral), mannitol (IV), isosorbide (oral)
Mechanism of Action:
Hyperosmotics are often only used during acute episodes of elevated IOP given their significant effects on other organ systems, and relatively transient nature of efficacy. They work to lower IOP by increasing blood osmolality which osmotically draws water from the vitreous cavity (Tenny et al, 2019).
Efficacy:
These systemic medications are very effective for short term IOP reduction. One study found IOP reduction of 19% at 15 min after IV mannitol administration, and reduction of 8% at four hours (Takkar et al, 2016). However, they should only be used acutely because their IOP lowering effects are transient, and become less effective over time (Schacknow et al, 2010).
Adverse Effects:
o Adverse effects include headache, confusion, backache, acute CHF, MI, subdural and subarachnoid hemorrhages, hyperglycemia and ketoacidosis in diabetics, and renal failure (Schacknow et al, 2010).
Other Considerations:
o Isosorbide is safer in diabetics compared to glycerin because glycerin is metabolized to glucose.
o Mannitol administered intravenously is more likely to cause cardiac side effects compared to oral glycerin or isosorbide (Schacknow et al, 2010.
o Due to the propensity for electrolyte disturbances, hyperosmotics are contraindicated in patients in with kidney failure and should be used with caution in elderly patients (Schacknow et al, 2010).
Fixed Combinations: Dorzolamide/timolol, brimonidine/timolol, brinzolamide/brimonidine, brinzolamide/timolol, bimatoprost/timolol, travoprost/timolol, tafluprost/tiolol, latunoprost/timolol
Mechanism of Action:
For many patients with ocular hypertension and glaucoma, a single IOP lowering medication is insufficient to achieve an adequate reduction in IOP, requiring additional medications to be prescribed to achieve goal IOP. Fixed combinations combine two classes of IOP lowering medication in a single bottle. With fixed combinations, patients require fewer bottles and oftentimes fewer dosages of medication per day. This offers a more convenient regimen and likely leads to better adherence (Olthoff et al, 2005). In addition, depending on the healthcare system, patient cost may be lessened with fixed combinations given that a copay may be required for only one medication rather than two (Higginbotham et al, 2010).
Efficacy:
In addition to the improved adherence, efficacy is also likely enhanced with fixed combination medications, as there is no need to wait between instillation of separate medications and thus no possibility of washout (Higginbotham et al, 2010).
Adverse Effects:
o Local adverse effects may be lessened with fixed combinations given reduction in dosage of medication and thus reduction in exposure to preservatives.
o Systemic adverse effects of fixed combinations are largely the same as that for the individual medication components.
Other Considerations:
o The downside of fixed combinations is the inability to change medication concentration or dosing schedule for individual medications (Higginbotham et al, 2010).
TREATMENT APPROACH BY PATIENT
o Age
o Pediatric population
§ Alpha agonists should be avoided in infants and young children, particularly in children under 6 years of age and weighing less than 20 kilograms, due to the risk of CNS depression (Arthur et al, 2011).
§ Beta blockers should be avoided in premature or small for age infants, as well as children with reactive airways (Freedman et al, 2006).
o Elderly population
§ Elderly patients have a greater number of comorbidities which should be taken into account when considering the potential adverse effects of an IOP lowering medication. However, age itself should also be considered given the increase in orthostatic hypotension and impotence with age - factors which may limit beta blocker use.
o Pregnancy (pre and post-partum)
o Pregnancy:
§ In 1979, a 5-letter system was introduced by the Food and Drug Administration (FDA) in the United States to indicate the risk of medication of causing birth defects if used during pregnancy. Category A is deemed safe, category B is possibly safe to use, category C has shown adverse effects in animal studies, category D shows definite risks but possible benefits, and category X drugs show known fetal risk that are not outweighed by possible benefits (Sachdeva et al, 2009).
§ Pregnancy results in a natural reduction in IOP, however, in some women, treatment to lower IOP is still necessary to prevent progression of their disease (Qureshi, 1997).
§ First trimester: Given the high risk of drug-induced fetal teratogenicity during the first trimester, all topical IOP-lowering medications should be avoided during these months if possible. However, if topical treatment is necessary, brimonidine may be the safest option during the first trimester, though it is still only a Category B medication. There are not yet human studies on the effects of rho kinase inhibitors during pregnancy, but these may also be a Category B pending more clinical information (Belkin et al, 2019).
§ Second and third trimester: Brimonidine should be avoided during the third trimester due to its expression in breast milk, and the risk of CNS depression in newborns with ingestion. Other classes of mediation, though all are Category C, can potentially be restarted during the second and third trimester as the risk of drug-induced fetal teratogenicity is much less (Belkin et al, 2019).
· Beta blockers should be monitored closely due to potential to dangerously lower fetal heart rate.
· Prostaglandin analogs may increase the risk of premature labor, especially when used in the third trimester and should be avoided for this reason (Sethi et al, 2016).
o Post-partum: Carbonic anhydrase inhibitors and beta blockers are approved for use when nursing, while alpha agonists are contraindicated during this time period due to the risk of CNS depression in newborns (Belkin et al, 2019).
o Adherence difficulty
o The least complicated eye drop regimen often promotes the greatest adherence as mentioned previously. In patients who have difficulty remembering or difficulty administering eye drops, a once a day regimen such as that used with prostaglandin analogs or a fixed combination is ideal. However, non-medical therapies such as incisional surgery and laser procedures should also be considered in patients with difficulty administering their IOP-lowering medications.
o Comorbidities:
o Obstructive pulmonary disease and uncontrolled asthma: Beta blockers should generally be avoided due adverse effect of antagonism of β-2 receptors on bronchial smooth muscle and exacerbation of obstructive lung disease (Ofner et al, 1987). However, their use can be considered in well controlled pulmonary disease and with appropriate patient education and cautioning.
o Hepatic disease: avoid oral carbonic anhydrase inhibitors due to risk of hyperammonemia (Bartlett, 2013).
o Renal insufficiency: avoid oral carbonic anhydrase inhibitors and hyperosmotics (Bartlett, 2013).
o Sulfa allergy: avoid oral carbonic anhydrase inhibitors due to risk of cross-reactivity. However, due to limited systemic absorption, topicals can often be employed with proper patient education.
o Bradycardia: avoid beta blockers due to risk of worsening bradycardia, heart block.
o Brittle diabetics: avoid beta blockers due to risk of masking effects of hypoglycemia, avoid hyperosmotic agents due to risk of hyperglycemia and ketoacidosis.
o Sexual dysfunction: avoid beta blockers and oral carbonic anhydrase inhibitors due to risk of impotence, worsened sexual dysfunction.
o Sickle cell trait, sickle cell anemia: avoid use of carbonic anhydrase inhibitors due to increase in sickling of erythrocytes with use (Bartlett, 2013).
o Unilateral disease
o Though not an absolute contraindication, consider avoiding prostaglandin analogs in unilateral disease due to propensity to cause periorbital fat atrophy, hypertrichosis and hyperpigmentation of eyelashes, darkening of irides, darkening of the eyelids.
o Ocular surface disease, BAK-sensitivity
o The use of preservative in eye drop formulations extends the shelf life considerably. The most common preservative in use is BAK, a soap-like quaternary ammonium found in approximately 70% of eye drops, which acts as a detergent by lysing cell membranes. BAK is known to cause a host of ocular adverse effects including tear film instability, loss of goblet cells, conjunctival squamous metaplasia, and disruption of the corneal epithelium (Baudouin et al, 2010). Polyquaternium-1 (Polyquad) is also a quaternary ammonium preservative but is much larger than BAK and not internalized by the corneal epithelium, and thus better tolerated than BAK (Steven et al, 2018). Stabalized Oxychloro Complex (SOC) is a combination of chlorine, chlorite, and chlorate found in brimonidine tartrate, which demonstrates antimicrobial activity through oxidation of intracellular lipids and glutathione. SofZia is an ionic buffer found in travoprost, and composed of boric acid, propylene glycol, sorbitol, and zinc chloride. Both SOC and SofZia are typically better tolerated than medications preserved with BAK (Yu et al, 2014; Rolando et al, 2011).
o Preservative free or at least BAK-free alternatives should be considered in patients with ocular polypharmacy (more than 1-2 medications per day) or those with ocular surface disease. Preservative-free medications are formulated into single use vials rather than multi-use bottles.
o BAK-free formulations include: latanoprost, travoprost, tafluoprost, timolol, dorzolamide, brimonidine, dorzolamide/timolol, bimatoprost/timolol, tafluprost/timolol
1. Addis, V. M., & Miller, E. (2018). Latanoprostene bunod ophthalmic solution 0.024% in the treatment of open-angle glaucoma: Design, development, and place in therapy. Clinical Ophthalmology, Volume 12, 2649-2657. https://doi.org/10.2147/opth.s156038
2. Aronson, J. K. (2011). Chapter 21. Diuretics. In Side effects of drugs annual: A worldwide yearly survey of new data and trends in adverse drug reactions. Elsevier.
3. Arthur, S., & Cantor, L. B. (2011). Update on the role of Alpha-agonists in glaucoma management. Experimental Eye Research, 93(3), 271-283. https://doi.org/10.1016/j.exer.2011.04.002
4. Bahler, C. K., Howell, K. G., Hann, C. R., Fautsch, M. P., & Johnson, D. H. (2008). Prostaglandins increase trabecular meshwork outflow facility in cultured human anterior segments. American journal of ophthalmology, 145(1), 114–119. https://doi.org/10.1016/j.ajo.2007.09.001
5. Bartels, S. P., Lee, S. R., & Neufeld, A. H. (1987). The effects of forskolin on cyclic AMP, intraocular pressure and aqueous humor formation in rabbits. Current Eye Research, 6(2), 307-320. https://doi.org/10.3109/02713688709025183
6. Bartlett, J. D. (2013). Inhibitors of Aqueous Formation. In Clinical ocular pharmacology (p. 260-261). Elsevier.
7. Baudouin, C., Labbé, A., Liang, H., Pauly, A., & Brignole-Baudouin, F. (2010). Preservatives in eyedrops: The good, the bad and the ugly. Progress in Retinal and Eye Research, 29(4), 312-334. https://doi.org/10.1016/j.preteyeres.2010.03.001
8. Belkin, A., Chen, T., DeOliveria, A. R., Johnson, S. M., Ramulu, P. Y., & Buys, Y. M. (2020). A practical guide to the pregnant and breastfeeding patient with glaucoma. Ophthalmology Glaucoma, 3(2), 79-89. https://doi.org/10.1016/j.ogla.2019.12.004
9. Boger, W. P. (1983). Shortterm “escape” and longterm “drift.”. The dissipation effects of the beta adrenergic blocking agents. Survey of Ophthalmology, 28, 235-240. https://doi.org/10.1016/0039-6257(83)90138-8
10. Cavet, M. E., & DeCory, H. H. (2018). The role of nitric oxide in the Intraocular pressure lowering efficacy of Latanoprostene Bunod: Review of nonclinical studies. Journal of Ocular Pharmacology and Therapeutics, 34(1-2), 52-60. https://doi.org/10.1089/jop.2016.0188
11. Danias, J., & Podos, S.M. Comparison of glaucomatous progression between untreated patients with normal-tension glaucoma and patients with therapeutically reduced intraocular pressures. (1999). American Journal of Ophthalmology, 126(4), 487-497. https://doi.org/10.1016/s0002-9394(98)00223-2
12. Dave, P., Villarreal, G., Friedman, D. S., Kahook, M. Y., & Ramulu, P. Y. (2015). Ability of bottle cap color to facilitate accurate patient–physician communication regarding medication identity in patients with glaucoma. Ophthalmology, 122(12), 2373-2379. https://doi.org/10.1016/j.ophtha.2015.06.013
13. Delamere, N. A. (2005). Ciliary body and ciliary epithelium. Advances in Organ Biology, 127-148. https://doi.org/10.1016/s1569-2590(05)10005-6
14. Detry-Morel, M. (2006). Side effects of glaucoma medications. Bulletin de la Societe Belge d'Ophtalmologie, 299, 27-40.
15. Docherty, J. R. (2009). Subtypes of functional α1-adrenoceptor. Cellular and Molecular Life Sciences, 67(3), 405-417. https://doi.org/10.1007/s00018-009-0174-4
16. Drance, S. M. (1974). Pilocarpine and Intraocular pressure. Archives of Ophthalmology, 91(2), 104. https://doi.org/10.1001/archopht.1974.03900060110004
17. Dubiner, H. B., Hill, R., Kaufman, H., Keates, E. U., Zimmerman, T. J., Mandell, A. I., Mundorf, T. K., Bahr, R. L., Schwartz, L. W., Towey, A. W., Hurvitz, L. M., Starita, R. J., Sassani, J. W., Ropo, A., Gunn, R., & Stewart, W. C. (1996). Timolol Hemihydrate vs Timolol maleate to treat ocular hypertension and open-angle glaucoma. American Journal of Ophthalmology, 121(5), 522-528. https://doi.org/10.1016/s0002-9394(14)75426-1
18. Freedman, S. F., & Johnston, S. C. (2006). Glaucoma in infancy and early childhood. Pediatric Ophthalmology, 345-374. https://doi.org/10.1007/978-3-540-68632-3_24
19. Friedman DS, Hahn SR, Gelb L, Tan J, Shah SN, Kim EE, Zimmerman TJ, Quigley HA. Doctor-patient communication, health-related beliefs, and adherence in glaucoma results from the Glaucoma Adherence and Persistency Study. Ophthalmology. 2008 Aug;115(8):1320-7, 1327.e1-3. doi: 10.1016/j.ophtha.2007.11.023. Epub 2008 Mar 5.
20. Frishman, W. H., & Covey, S. (1990). Penbutolol and Carteolol: Two new beta-adrenergic blockers with partial Agonism. The Journal of Clinical Pharmacology, 30(5), 412-421. https://doi.org/10.1002/j.1552-4604.1990.tb03479.x
21. Garway-Heath, D. F., Lascaratos, G., Burton, R., Bunce, C., Xing, W., Crabb, D. P., Russell, R. A., & Shah, A. (2013). The United Kingdom glaucoma treatment study: A multicenter, randomized, double-masked, placebo-controlled trial. Ophthalmology, 120(12), 2540-2545. https://doi.org/10.1016/j.ophtha.2013.07.054
22. Gaton, D. D. (2001). Increased matrix Metalloproteinases 1, 2, and 3 in the monkey Uveoscleral outflow pathway after topical prostaglandin f2α–isopropyl ester treatment. Archives of Ophthalmology, 119(8), 1165. https://doi.org/10.1001/archopht.119.8.1165
23. Goel, M. (2010). Aqueous humor dynamics: A review. The Open Ophthalmology Journal, 4(1), 52-59. https://doi.org/10.2174/1874364101004010052
24. Higginbotham. (2009). Considerations in glaucoma therapy: Fixed combinations versus their component medications. Clinical Ophthalmology, 1. doi:10.2147/opth.s6645
25. Kass, M. A., Heuer, D. K., & Higginbotham, E. J. (2002). The ocular hypertension treatment study. Archives of Ophthalmology, 120(6), 701. https://doi.org/10.1001/archopht.120.6.701
26. Khawaja, A. P., Chan, M. P., Broadway, D. C., Garway-Heath, D. F., Luben, R., Yip, J. L., Hayat, S., Wareham, N. J., Khaw, K., & Foster, P. J. (2014). Systemic medication and Intraocular pressure in a British population. Ophthalmology, 121(8), 1501-1507. https://doi.org/10.1016/j.ophtha.2014.02.009
27. KOBAYASHI, M., & NAITO, K. (2000). Pharmacological profiles of the potent carbonic anhydrase inhibitor dorzolamide hydrochloride, a topical antiglaucoma agent. Folia Pharmacologica Japonica, 115(6), 323-328. https://doi.org/10.1254/fpj.115.323
28. Lacey, J., Cate, H., & Broadway, D. C. (2008). Barriers to adherence with glaucoma medications: A qualitative research study. Eye, 23(4), 924-932. https://doi.org/10.1038/eye.2008.103
29. Lu, L. J., Tsai, J. C., & Liu, J. (2017). Novel Pharmacologic Candidates for Treatment of Primary Open-Angle Glaucoma. The Yale journal of biology and medicine, 90(1), 111–118.
30. Lütjen-Drecoll, E., & Tamm, E. (1988). Morphological study of the anterior segment of cynomolgus monkey eyes following treatment with prostaglandin F2α. Experimental Eye Research, 47(5), 761-769. https://doi.org/10.1016/0014-4835(88)90043-7
31. Mansouri, K., Iliev, M. E., Rohrer, K., & Shaarawy, T. (2011). Compliance and knowledge about glaucoma in patients at tertiary glaucoma units. International Ophthalmology, 31(5), 369-376. https://doi.org/10.1007/s10792-011-9468-2
32. Marando, C. M., Seibold, L. K., SooHoo, J. R., Pantcheva, M. B., Ramulu, P. Y., & Kahook, M. Y. (2015). The utility of cap color and bottle characteristics for topical glaucoma therapy. Ophthalmology, 122(12), 2577-2578. https://doi.org/10.1016/j.ophtha.2015.04.039
33. Maren, T. H. (1967). Carbonic anhydrase: Chemistry, physiology, and inhibition. Physiological Reviews, 47(4), 595-781. https://doi.org/10.1152/physrev.1967.47.4.595
34. Maus, T. L. (1997). Comparison of Dorzolamide and Acetazolamide as suppressors of aqueous humor flow in humans. Archives of Ophthalmology, 115(1), 45. https://doi.org/10.1001/archopht.1997.01100150047008
35. Mehran, N. A., Sinha, S., & Razeghinejad, R. (2019). New glaucoma medications: Latanoprostene bunod, netarsudil, and fixed combination netarsudil-latanoprost. Eye, 34(1), 72-88. https://doi.org/10.1038/s41433-019-0671-0
36. Moshirfar, M., Parker, L., Birdsong, O. C., Ronquillo, Y. C., Hofstedt, D., Shah, T. J., Gomez, A. T., & Hoopes, P. (2018). Use of Rho kinase Inhibitors in Ophthalmology: A Review of the Literature. Medical hypothesis, discovery & innovation ophthalmology journal, 7(3), 101–111.
37. Neufeld, A. H., Jampol, L. M., & Sears, M. L. (1972). Cyclic-AMP in the aqueous humor: The effects of adrenergic agents. Experimental Eye Research, 14(3), 242-250. https://doi.org/10.1016/0014-4835(72)90009-7
38. Ofner, S., & Smith, T. J. (1987). Betaxolol in chronic obstructive pulmonary disease. Journal of Ocular Pharmacology and Therapeutics, 3(2), 171-176. doi:10.1089/jop.1987.3.171
39. Olthoff, C., Schouten, J., Vandeborne, B., & Webers, C. (2005). Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular HypertensionAn evidence-based review. Ophthalmology, 112(6), 953-961.e7. https://doi.org/10.1016/j.ophtha.2004.12.035
40. Orzalesi, N., Rossetti, L., Invernizzi, T., Bottoli, A., & Autelitano, A. (2000). Effect of timolol, latanoprost, and dorzolamide on circadian IOP in glaucoma or ocular hypertension11Edited by Thomas J. Liesegang, MD. American Journal of Ophthalmology, 130(5), 686. https://doi.org/10.1016/s0002-9394(00)00751-0
41. Parrish, R. K., Palmberg, P., & Sheu, W. (2003). A comparison of latanoprost, bimatoprost, and travoprost in patients with elevated intraocular pressure:. American Journal of Ophthalmology, 135(5), 688-703. https://doi.org/10.1016/s0002-9394(03)00098-9
42. Pollack, I. P., Brown, R. H., Crandall, A. S., Robin, A. L., Stewart, R. H., & White, G. L. (1988). Prevention of the rise in Intraocular pressure following Neodymium-YAG posterior Capsulotomy using topical 1% Apraclonidine. Archives of Ophthalmology, 106(6), 754-757. https://doi.org/10.1001/archopht.1988.01060130824031
43. Qureshi IA. Intraocular pressure and pregnancy: a comparison between normal and ocular hypertensive subjects. Archives of Medical Research. 1997 ;28(3):397-400.
44. Ramakrishan, R., Robin, A. L., & Khurana, M. (2013). 42. Medical Management of Glaucoma. In Diagnosis and management of glaucoma (p. 479). JP Medical.
45. Reitsamer, H., Posey, M., & Kiel, J. (2006). Effects of a topical α2 adrenergic agonist on ciliary blood flow and aqueous production in rabbits. Experimental Eye Research, 82(3), 405-415. https://doi.org/10.1016/j.exer.2005.07.015
46. Robin, A., & Covert, D. (2005). Does adjunctive glaucoma therapy affect adherence to the initial primary therapy? Ophthalmology, 112(5), 863-868. https://doi.org/10.1016/j.ophtha.2004.12.026
47. Rolando, M., Crider, J. Y., & Kahook, M. Y. (2011). Ophthalmic preservatives: Focus on polyquaternium-1. Expert Opinion on Drug Delivery, 8(11), 1425-1438. https://doi.org/10.1517/17425247.2011.617736
48. Rosenberg, L. F., Krupin, T., Tang, L., Hong, P. H., & Ruderman, J. M. (1998). Combination of systemic acetazolamide and topical dorzolamide in reducing intraocular pressure and aqueous humor formation. Ophthalmology, 105(1), 88-93. https://doi.org/10.1016/s0161-6420(98)91421-x
49. Sachdeva, P., Patel, B. G., & Patel, B. K. (2009). Drug use in pregnancy; a point to ponder!. Indian journal of pharmaceutical sciences, 71(1), 1–7. https://doi.org/10.4103/0250-474X.51941
50. Sakamoto, E., Ishida, W., Sumi, T., Kishimoto, T., Tada, K., Fukuda, K., Yoneda, T., Kuroiwa, H., Terao, E., Fujisawa, Y., Nakakura, S., Jian, K., Okumichi, H., Kiuchi, Y., & Fukushima, A. (2019). Evaluation of offset of conjunctival hyperemia induced by a rho-kinase inhibitor; 0.4% Ripasudil ophthalmic solution clinical trial. Scientific Reports, 9(1). https://doi.org/10.1038/s41598-019-40255-9
51. Sambhara, D., & Aref, A. A. (2013). Glaucoma management: Relative value and place in therapy of available drug treatments. Therapeutic Advances in Chronic Disease, 5(1), 30-43. https://doi.org/10.1177/2040622313511286
52. Schacknow, P. N., & Samples, J. R. (2010). 51. Medications used to treat glaucoma. In The glaucoma book: A practical, evidence-based approach to patient care (p. 610). Springer Science & Business Media.
53. Schadlu, R. (1998). Comparison of the efficacy of Apraclonidine and Brimonidine as aqueous suppressants in humans. Archives of Ophthalmology, 116(11), 1441. https://doi.org/10.1001/archopht.116.11.1441
54. Schlotzer-Schrehardt U, Zenkel M, Nüsing RM. Expression and localization of FP and EP prostanoid receptor subtypes in human ocular tissues. Invest Ophthalmol Vis Sci. 2002;43:1475–1487.
55. Serle, J. B., Katz, L. J., McLaurin, E., Heah, T., Ramirez-Davis, N., Usner, D. W., Novack, G. D., & Kopczynski, C. C. (2018). Two phase 3 clinical trials comparing the safety and efficacy of Netarsudil to Timolol in patients with elevated Intraocular pressure: Rho kinase elevated IOP treatment trial 1 and 2 (ROCKET-1 and ROCKET-2). American Journal of Ophthalmology, 186, 116-127. https://doi.org/10.1016/j.ajo.2017.11.019
56. Sethi, H. D., Naik, M., & Gupta, V. S. (2016). Management of glaucoma in pregnancy: Risks or choices, a dilemma? International Journal of Ophthalmology. https://doi.org/10.18240/ijo.2016.11.24
57. Shaw, P. X., Sang, A., Wang, Y., Ho, D., Douglas, C., Dia, L., & Goldberg, J. L. (2017). Topical administration of a rock/Net inhibitor promotes retinal ganglion cell survival and axon regeneration after optic nerve injury. Experimental Eye Research, 158, 33-42. https://doi.org/10.1016/j.exer.2016.07.006
58. Shin, J., & Johnson, J. A. (2007). Pharmacogenetics of beta-blockers. Pharmacotherapy, 27(6), 874–887. https://doi.org/10.1592/phco.27.6.874
59. Shiroma, L. O., & Costa, V. P. (2015). Parasympathomimetics. Glaucoma, 577-582. https://doi.org/10.1016/b978-0-7020-5193-7.00056-x
60. Sly, W. S., & Hu, P. Y. (1995). Human carbonic Anhydrases and carbonic Anhydrase deficiencies. Annual Review of Biochemistry, 64(1), 375-401. https://doi.org/10.1146/annurev.bi.64.070195.002111
61. Soll, D. B. (1980). Evaluation of Timolol in chronic open-angle glaucoma. Archives of Ophthalmology, 98(12), 2178. https://doi.org/10.1001/archopht.1980.01020041030004
62. SooHoo, J. R., Golas, L., Marando, C. M., Seibold, L. K., Pantcheva, M. B., Ramulu, P. Y., & Kahook, M. Y. (2016). Glaucoma patient treatment preferences. Ophthalmology, 123(7), 1621-1622. https://doi.org/10.1016/j.ophtha.2016.01.018
63. Steven, D. W., Alaghband, P., & Lim, K. S. (2018). Preservatives in glaucoma medication. British Journal of Ophthalmology, 102(11), 1497-1503. https://doi.org/10.1136/bjophthalmol-2017-311544
64. Stewart, R. H. (1986). Betaxolol vs Timolol. Archives of Ophthalmology, 104(1), 46. https://doi.org/10.1001/archopht.1986.01050130056019
65. Stewart, W. C., Konstas, A. G., Nelson, L. A., & Kruft, B. (2008). Meta-analysis of 24-Hour Intraocular pressure studies evaluating the efficacy of glaucoma medicines. Ophthalmology, 115(7), 1117-1122.e1. https://doi.org/10.1016/j.ophtha.2007.10.004
66. Stryker, J. E., Beck, A. D., Primo, S. A., Echt, K. V., Bundy, L., Pretorius, G. C., & Glanz, K. (2010). An exploratory study of factors influencing glaucoma treatment adherence. Journal of Glaucoma, 19(1), 66-72. doi:10.1097/ijg.0b013e31819c4679
67. Takkar, B., Chandra, P., Shah, R., Bhatia, I., Roy, S., & Sihota, R. (2016). Effect of intravenous mannitol on Intraocular pressure in Vitrectomized silicone-oil-Filled eyes. Seminars in Ophthalmology, 32(6), 672-675. https://doi.org/10.3109/08820538.2016.1169301
68. Tanna, A. P., & Johnson, M. (2018). Rho kinase inhibitors as a novel treatment for glaucoma and ocular hypertension. Ophthalmology, 125(11), 1741-1756. https://doi.org/10.1016/j.ophtha.2018.04.040
69. Taylor, M. Pharmacogenetics of the human beta-adrenergic receptors.Pharmacogenomics J 7, 29–37 (2007). https://doi.org/10.1038/sj.tpj.6500393
70. Tenny S, Patel R, Thorell W. Mannitol. [Updated 2019 Dec 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470392/
71. Tu, E. Y. (2014). Balancing antimicrobial efficacy and toxicity of currently available topical ophthalmic preservatives. Saudi Journal of Ophthalmology, 28(3), 182-187. doi:10.1016/j.sjopt.2014.06.006
72. Van der Valk, R., Webers, C. A., Schouten, J. S., Zeegers, M. P., Hendrikse, F., & Prins, M. H. (2005). Intraocular pressure–lowering effects of all commonly used glaucoma drugs. Ophthalmology, 112(7), 1177-1185. https://doi.org/10.1016/j.ophtha.2005.01.042
73. Walters, T. R. (1996). Development and use of brimonidine in treating acute and chronic elevations of intraocular pressure: A review of safety, efficacy, dose response, and dosing studies. Survey of Ophthalmology, 41, S19-S26. https://doi.org/10.1016/s0039-6257(96)82028-5
74. Wand, M., & Gilbert, C. M. (1999). Latanoprost and herpes simplex keratitis. Journal of Glaucoma, 8(Supplement 1), S1. https://doi.org/10.1097/00061198-199902001-00002
75. Watson, P. G. (2001). A 7 year prospective comparative study of three topical beta blockers in the management of primary open angle glaucoma. British Journal of Ophthalmology, 85(8), 962-968. https://doi.org/10.1136/bjo.85.8.962
76. Webb, N. (2018). Tachyphylaxis. In J. Kreutzer, J. DeLuca, & B. Caplan (Eds.), Encyclopedia of clinical neuropsychology. Springer.
77. Wheeler, L., & Woldemussie, E. (2001). Alpha-2 adrenergic receptor agonists are Neuroprotective in experimental models of glaucoma. European Journal of Ophthalmology, 11(2_suppl), 30-35. https://doi.org/10.1177/112067210101102s03
78. Winkler, N. S., & Fautsch, M. P. (2014). Effects of prostaglandin analogues on aqueous humor outflow pathways. Journal of Ocular Pharmacology and Therapeutics, 30(2-3), 102-109. https://doi.org/10.1089/jop.2013.0179