Uveitis-Glaucoma-Hyphema Syndrome
| Primary authors |
|
|---|
Uveitis-Glaucoma-Hyphema Syndrome
Lecture Video: https://youtu.be/vF2DtQ24R-0
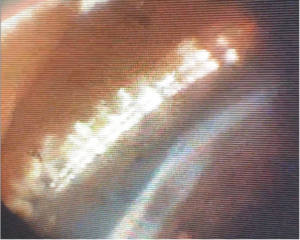
Uveitis-Glaucoma-Hyphema (UGH) Syndrome is a secondary inflammatory glaucoma classically related to an intraocular lens (IOL) haptic and/or optic rubbing on anterior chamber uveal and vascular structures, frequently involving the posterior surface of the iris and surrounding tissues. UGH syndrome is more likely to occur when squared edged haptics (a design feature of most single piece acrylic lenses commercialized today) are placed in the sulcus (Figure 1) when compared to rounded PMMA, PVDF or Polypropylene haptics which are used in 3-piece IOL designs. UGH syndrome may also be associated with poorly sized anterior chamber IOLs and iris or scleral fixated IOLs when the haptics come in direct contact with the posterior surface of the iris, iris root and vascular tissues proximate to the sulcus. With anterior chamber IOLs, remember that the proper size for the lens is obtained by using the horizontal corneal white-to-white distance and adding 1mm. More recently, cosmetic iris implants have been implicated in causing UGH syndrome due to poor surgical technique, apposition of the implant against the iris and poor design that contributes to devices chaffing the iris and surrounding vascular tissues. It is important to note that in-the-bag IOLs may also cause UGH when the bag is unstable allowing for contact with surrounding tissues.
Clinical Findings
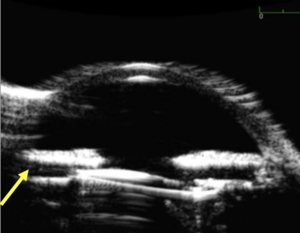
UGH syndrome is classically associated with the triad of chronic inflammation, recurrent bleeding and iris transillumination defects. Elevated intraocular pressure (IOP) is noted with advancing dysfunction of the trabecular meshwork (TM) and is occasionally associated with iris neovascularization and cystoid macular edema. The patient may present with complaints of episodic blurring of vision (repeated hyphemas) photophobia, red eye and pain. Ultrasound biomicroscopy (UBM) is helpful to determine position of the IOL since the points of interest (haptic-iris-sulcus relationship) are often not visible on slit lamp exam (Figure 2). It is important to note that UBM can often indicate apposition of the haptic and/or optic against specific ocular structures (like the iris) but is not definitive evidence that the lens is outside of the capsular bag (since capsular bag stability may be compromised and allowing for tilting and contact with adjacent structures). Gonioscopy is essential to determine presence of blood that may not be visible without direct view of the angle. The level of angle pigmentation (look for distribution of pigment in all quadrants and examine meticulously for any possible tumors that may mimic UGH syndrome) should also be noted (Figure 3). Gonioscopy can also identify points of contact between the haptics and the iris which appear as anterior outpouchings of iris tissue. Gonioscopy is also key to identify any neovascularization of the iris or angle, which can be a feature of chronic UGH syndrome but may also indicate presence of neovascular glaucoma from ischemic processes (which can mimic UGH syndrome) unrelated to IOL position. Elevation of IOP can occur due to all factors noted above with both physical plugging of the TM (from pigment, blood and inflammatory cells) as well as direct mechanical destruction of the TM from compression and/or rubbing against IOL structures.
Differential Diagnosis
1. Uveitic Glaucomas
2. Traumatic Hyphema
3. Neovascular Glaucoma
4. Anterior Segment Tumors
5. Pigment Dispersion Glaucoma
Treatment
Practice pattern changes with shifting from anterior to posterior chamber IOLs, enhanced IOL haptic and optic design features, use of modern acrylic materials and improved surgical techniques have all led to a decrease in incidence of UGH syndrome post cataract surgery with IOL implantation (from ~3% to ~0.4%). Treatment includes IOP lowering medications (avoid miotics which can increase contact between the iris and the IOL), steroids to treat inflammation plus or minus NSAIDs especially when cystoid macular edema is present. The definitive treatment involves surgical repositioning or exchange of the IOL. Concomitant glaucoma surgery (angle based or filtration) may also be used when the glaucoma is advanced, and the outflow system of the eye is too severely compromised to recover with just addressing the IOL issues at hand. Combining glaucoma surgery with IOL repositioning/exchange is often a hard issue to address and must consider the specific patient as well as the overall staging of glaucoma along with clinical examination of the angle to ascertain likelihood of the drainage system recovering over time.
Further reading
1. Apple DJ, Mamlis N, Loftfield K, Googe JM, Novak LC, Kavka-van Norman D, Brady SE, Olson RJ. Complications of Intraocular Lenses. A Historical and Histopathological Review. Surv Ophthalmol 1984;29:1-54. 2. Arthur SN, Wright MM, Krammarevsky N, Kaufman SC, Grajewski AL. Uveitis-Glucoma-Hyphema Syndrome and Corneal Decompensation in Association with Cosmetic Iris Implants. Am J Ophthalmology 2009;148:790-3.