Concomitant Glaucoma Drainage Devices and Corneal Transplantation
| Primary authors |
|
|---|
A number of conditions may necessitate combined corneal transplantation and implantation of a glaucoma drainage device. Conditions such as trauma, iridocorneal endothelial (ICE) syndrome, herpetic infection, aphakia, or neovascular glaucoma are commonly associated with elevated intraocular pressure (IOP) and corneal scar or decompensation. The anterior segment procedures can be performed in combination by a glaucoma and corneal surgeon or simultaneously by a single anterior segment surgeon. It is important for the surgeon to determine preoperatively the risk of elevated IOP after keratoplasty. The risk of glaucoma after keratoplasty depends on the indication for corneal transplant; patients with keratoconus or Fuchs’ dystrophy have been found to have significantly less postoperative glaucoma than patients with corneal ulcer, herpetic disease, and aphakia.
Preoperative Considerations
Corneal graft survival and maximization of visual potential are intimately tied to adequate IOP control. In a patient undergoing corneal transplantation, a comprehensive evaluation prior to surgery is necessary to determine whether a combined surgery is the best option for the patient. Glaucoma surgery for uncontrolled IOP usually takes precedence over the corneal trans-plant because the damage that occurs with glaucoma is irreversible. Glaucoma surgery almost always can be performed first while delaying the cornea trans-plantation; the exception is corneal melt or perforated cornea in which the cornea transplantation becomes urgent. If the progression of glaucoma can be arrested, the surgeon can safely come back at a later time and perform corneal transplantation. This staged procedure has the potential to increase the success rate for both surgeries, as there is adequate pressure control at the time of transplantation and less overall inflammation; however, outcomes of staged vs combined surgeries have been variable in the literature. Ultimately, the decision between staged vs combined glaucoma and transplant surgery is deter-mined by the surgeon and patient. In some situations, such as in a patient with severely uncontrolled preoperative IOP, poor medication compliance, medical contraindications to multiple surgeries, or in very controlled situations such as an ICE syndrome in which the eye is not in an inflamed state, one may prefer to perform combined glaucoma and corneal transplant surgery. In most cases, glaucoma drainage devices (GDDs) are preferable over trabeculectomy generally because of the increased inflammatory reaction present following corneal transplantation, which could lead to bleb failure.
Descemet’s Stripping Endothelial Keratoplasty Combined With Glaucoma Drainage Device
Performing combined GDD implantation and Descemet’s stripping endothelial keratoplasty (DSEK) is possible in patients who have endothelial dysfunction and uncontrolled glaucoma. One reason for combining this procedure is in patients with ICE syndrome who have abnormal endothelial cell function and deterioration of the angle and trabecular meshwork. Fur-ther, certain patients with Fuchs’ dystrophy who have combined endothelial dysfunction and uncontrolled IOP may also be good candidates for this procedure because elevated IOP can increase corneal edema and decrease the quality of vision.
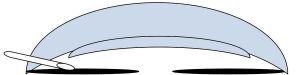
The first step in a combined DSEK and glaucoma surgery should be implantation of the GDD. The rationale for placing the glaucoma implant first is that it is easier to suture the GDD plate to the sclera on a relatively firm eye. Additionally, the insertion of the tube into the anterior chamber would likely cause a collapse of the anterior chamber or detachment of the DSEK lenticule, thus the DSEK should be performed after the GDD por-tion of the surgery is completed (see Chapter 8 for a complete description of the surgery). Similar to the standard GDD implantation procedure, after securing the plate, the tube is cut to the appropriate length and inserted into the eye. It is very important in the combined surgery to ensure that the tube is cut to the appropriate length and is angled in the iris plane or directed slightly posteriorly. The intraocular portion of the tube should be trimmed relatively short to prevent it from interfering with graft insertion and from chronically touching the corneal transplant, which would cause it to decompensate (Figure 37-1). A patch graft of sclera or pericardium should be secured over the tube, and the conjunctiva can be repositioned and fastened with sutures.
Next, viscoelastic is inserted into the anterior chamber; then Descemet’s membrane can be scored, stripped, and removed from the eye. An inferior peripheral iridotomy is used by some surgeons to prevent pupillary block from the air bubble that will be placed in the anterior chamber. The inferior peripheral iridotomy also allows the surgeon to leave a relatively large air bubble, which can be advantageous for increased air tamponade of the graft to the stroma or in patients in whom air escape is anticipated (aphakia, trabeculectomy, and/or patent tube shunt present preoperatively). The inferior peripheral iridotomy can be created prior to removal of the viscoelastic with microforceps and microscissors, or preoperatively with the YAG laser. A 4- to 5-mm clear corneal or scleral tunnel incision should be created approximately 90 degrees away from the insertion of the glaucoma tube. The viscoelastic is removed and the corneal transplant tissue cut to the appropriate size. Once the DSEK lenticule is separated from the rest of the corneal tissue, it can be inserted into the anterior chamber using an insertion device or tissue forceps. The graft is unfolded in the anterior chamber with balanced salt solution and an air bubble. The graft is positioned into place, and then a large air bubble is instilled into the anterior chamber. Air bubble management can be challenging in patients with a preexisting GDD, given the propensity for air to rise and escape through the tube. In a combined procedure, because the tube is typically tied off or valved, air does not go through the GDD. However, if this is a problem, viscoelastic can be inserted into the tip of the tube to help provide a temporary plug so pressure can be maintained to facilitate DSEK graft attachment. A large air bubble can either be left in place with an inferior iridotomy or can be exchanged for balanced salt solution after an appropriate period of time with a full air bubble. A full air bubble is a 100% fill of air in the anterior chamber, which is typically left in place for 8 to 10 minutes after graft insertion to facilitate adhesion of the donor lenticule to the host stroma. Then, the size of the air bubble is adjusted based on the surgical technique used (ie, only a small amount of air is exchanged with balanced salt solution if an inferior iridotomy is present and a large bubble of air is left) or about 50% of the air bubble is exchanged for balanced salt solution in the absence of an inferior peripheral iridotomy to avoid pupillary block.
Patients who have combined DSEK and glaucoma surgery often need to take topical steroids for at least 1 year. The prolonged steroid use can cause a rise in IOP, and this should be monitored closely. Additionally, as the bleb wall forms around the GDD plate, there can be a hypertensive phase between weeks 2 and 10, requiring the addition of topical medications. If glaucoma medications are needed in addition to the GDD to lower IOP, alpha-agonists or beta-blockers are typically the medications of choice. Prostaglandin analogues can increase the inflammatory response and increase the chance of corneal graft rejection, and carbonic anhydrase inhibitors can inhibit endothelial cell pump function, thereby limiting the effectiveness of the corneal graft.
Glaucoma Drainage Device in Combination With Penetrating Keratoplasty
Diseases that affect the corneal stroma or induce severe irregular astigmatism, such as scarring after trauma, infectious corneal ulcers, or herpetic infection, are better treated with full-thickness corneal transplant than DSEK. If the patient also has progressive glaucoma that is not controllable with medications, one could consider combined full-thickness cornea transplant with GDD implantation. The most common cause of a combined full-thickness corneal transplant and glaucoma surgery is trauma (although other causes, such as inflammatory conditions or herpetic keratouveitis, are also possible).
Again, the GDD should be performed first to facilitate securing the plate to the sclera. Given the increased risk of graft failure with a GDD, it is important to ensure that the intraocular portion of the glaucoma tube is directed away from the cornea and that it is not too long inside the eye. After the GDD is placed, the typical steps of a full-thickness cornea’ transplant can be performed. A vacuum trephine, the diameter of which depends on the location of the pathology present, is used to trephinate the host cornea. Similarly, a punch trephine is used to cut a corneal button of similar or slightly larger size to transplant into the host cornea. A 10-0 nylon suture is used in an interrupted and/or running fashion to secure the full-thickness corneal transplant to the host eye. Interrupted sutures are preferred in an inflammatory condition so that selective suture removal may be performed if any of the sutures become a source of inflammation. The postoperative period involves gradual visual recovery and requires topical steroids for an extended period of time. The IOP must be watched carefully during this period and treated appropriately. Again, prostaglandin and carbonic anhydrase inhibitors are ideally avoided because of the pro-inflammatory component of prostaglandin analogues and the decrease in endothelial cell pump function with carbonic anhydrase inhibitors.
Postoperative Considerations
The failure rate of glaucoma surgery and cornea transplantation is variable but can be higher in combined surgeries as mentioned previously. In some cases, the benefits of providing simultaneous surgery outweigh the risks of surgical failure. Postoperatively, both the glaucoma surgery and the corneal transplant need to be monitored for signs of failure. Corneal rejection is identified by intraocular cell and flare, keratic precipitates present on the endothelium, corneal edema, epithelial irregularity, or other signs such as a Khodadoust line. Glaucoma failure is determined predominantly by the morphology of the overlying bleb and the IOP. multiple glaucoma tubes can be placed in eyes with prior corneal transplantation should the IOP be inadequate. The risk of graft failure should be weighed against the risk of progressive glaucoma in this setting. Cycloab-lative procedures are also an option to achieve better IOP control without implantation of more hardware.
Special Considerations
In patients who have had a vitrectomy and need glaucoma surgery combined with a corneal transplant, it is advisable to place the GDD tube into the posterior segment to avoid all possibility of corneal decompensation secondary to the cornea–tube touch.
Conclusion
Corneal transplantation and glaucoma surgery can be performed concomitantly. Glaucoma surgery usually takes precedence over corneal transplantation because the damage caused by glaucoma is irreversible. In the setting of endothelial dysfunction, a DSEK combined with GDD is the preferred approach. If corneal scarring or irregular astigmatism is present, penetrating keratoplasty combined with GDD is typically performed. The majority of the glaucoma portion of the procedure is usually performed prior to entering the intraocular space. It is important to avoid endothelial tube touch, which can cause corneal decompensation. Managing postoperative inflammation is critical to the survival of both the corneal transplant and the glaucoma surgery.
Key Points
- Combined corneal transplantation and glaucoma surgery can be performed.
- Usually a GDD is combined with corneal transplantation.
- Avoiding endothelial tube touch is important to prevent corneal decompensation.
- Aggressively managing postoperative inflammation is critical for the success of the corneal transplant and glaucoma surgery.
Suggested Readings
Ayyala RS. Penetrating keratoplasty and glaucoma. Surv Ophthalmol. 2000;45(2):91-105. Lee RK, Fantes F. Surgical management of patients with combined glaucoma and corneal transplant surgery. Curr Opin Ophthalmol. 2003;14(2):95-99.
Price FW Jr, Price MO. Is it worthwhile to combine penetrating keratoplasty with glaucoma drainage implants? Cornea. 2008;27(3):261-262.