Glaucoma Drainage Device Implantation Combined With Pars Plana Vitrectomy
| Primary authors |
|
|---|
Typically, glaucoma drainage devices (GDDs) and pars plana vitrectomy (PPV) are combined when the drainage tube needs to be placed through the pars plana. Although there are multiple reasons why a tube would be placed through the pars plana instead of the anterior segment, there are roughly 3 broad categories: to protect compromised corneal endothelium, the anterior segment will not anatomically accept a tube, or perilimbal conjunctival thinning or scarring. Additionally, if a vitrectomy and a GDD are both required (ie, neovascular glaucoma with nonclearing vitreous haemorrhage), combining a PPV and GDD may be more convenient and lead to a better outcome than performing the surgeries separately.
Considerations for Combining Glaucoma Drainage Device and Pars Plana Vitrectomy
Reasons to Consider PPV and Pars Plana Tube Insertion
- Compromised corneal endothelium.
- Fuchs’ or pseudophakic bullous keratopathy.
- Corneal edema secondary to anterior chamber tube (ie, reposition tube into pars plana).
- Penetrating keratoplasty or endothelial graft.
- Anterior segment will not accept a tube.
- Extensive high peripheral anterior synechiae.
- Vitreous prolapse anteriorly/unicameral eyes.
- Unable to visualize anterior chamber for tube placement (ie, keratoprosthesis).
- Chronic anterior segment neovascularization (ie, hyphema could block tube).
- Very shallow anterior chamber.
- Ocular surface disorders.
- Extensive anterior/perilimbal conjunctival scarring or recession from previous surgery.
- Reposition eroded tube into pars plana.
- Complicated disease requiring simultaneous vitreoretinal and glaucoma surgery.
Effectively combining efforts requires that the vitreoretinal surgeon and the glaucoma surgeon communicate well and plan the surgery. important points to discuss include the following:
- Anesthesia. A combined PPV and tube insertion likely will be lon-ger and more involved than either procedure separately. Although retrobulbar block is appropriate for many patients, general anesthesia may be more appropriate for some.
- Location of the GDD. The planned location for GDD placement may affect placement of the PPV ports. If the vitrectomy is done with a 23-or 25-gauge system, one of the ports may be positioned so that it can be reused for tube insertion. Additionally, the vitreoretinal surgeon should be reminded to thoroughly trim the vitreous base, particularly in the planned quadrant for tube insertion.
- Opening conjunctiva. Many glaucoma doctors are quite particular about how the conjunctiva is handled, and this issue should be discussed with their vitreoretinal colleague. If a 20-gauge PPV is going to be performed, the extent and location of the peritomy should be planned to accommodate the GDD and the PPV sclerostomies. Even for 23- or 25-gauge vitrectomies that can be done transconjunctivally, the conjunctiva should be opened in the quadrant of the tube prior to placement of the trochars to avoid conjunctival holes.
- Order of surgical steps. Typically I begin the combined surgery by opening up the conjunctiva and securing the plate to the eye. The vitreoretinal specialist will then complete a PPV. Finally, I will insert the tube into the pars plana, secure the patch graft, and close the conjunctiva.
It may be more convenient or efficient for the vitreoretinal surgeon to perform the complete PPV first, thereby allowing the glaucoma specialist to follow and complete the entire tube implant surgery uninterrupted. However, the eye is often quite hypotonous immediately following the PPV, which can make placement of the plate more difficult.
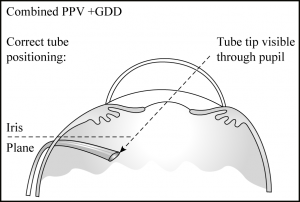
Pars Plana Tube Insertion
Placement of the tube through the pars plana is straightforward. The tube should be laid across the limbus and trimmed so that it extends approximately 2 - to 3-mm past the limbus. This technique should ensure adequate length so that the tube can be visualized postoperatively at the slit lamp. The tube is then trimmed with a posterior bevel so that if it rotates anteriorly, it will not become obstructed by iris. If an existing PPV port is not being utilized, a 23-gauge needle is used to make a sclerostomy tract, directing the needle parallel to, or slightly posterior to, the plane of the iris; if it is pointed too posteriorly, the tube may rarely “kink” at the sclerostomy. The sclerostomy should be created 3.5 to 4mm posterior to the limbus in pseudophakes and 4mm in phakic patients. The tube is then inserted and visually inspected through the pupil in the anterior vitreous cavity; rotating the eye toward the quadrant with the tube or gently depressing in the area of the tube entry can facilitate visualization (Figure 38-1). The tube is covered with donor sclera, and the conjunctiva closed with 8-0 Vicryl suture.
An alternative to placing the bare tube directly through the pars plana is to use a dedicated pars plana “knuckle” (Model: PC, New World Medical Inc). This device fits onto an existing tube and bends it gently, avoiding a kink. I have never found this device necessary, but if used, it should be covered with graft material.
Vitreous Incarceration
Vitreous incarceration is a complication that can occur at any time intra- or postoperatively. This complication is uncommon if the vitreoretinal surgeon is able to remove the majority of the vitreous body.
Vitreous blocking the tube may be recognized intraoperatively if fluid fails to pass through the tube after insertion. After the tube is inserted into the eye, I like to pressurize the anterior chamber before closing the conjunctiva and ensure that fluid is flowing through the tube (or through the fenestration slits if the tube is tied off) and that the eye pressure comes down as expected.
If vitreous blocks the tube postoperatively, an elevated intraocular pres-sure (IOP) and flat bleb will be noted. If the intraocular portion of the tube was left long enough to be visualized at the slit lamp, vitreous may be seen extending into the tube. YAG laser vitreolysis can be successful in restoring tube function. If the tube cannot be visualized, or if YAG laser is unsuccessful, a repeat PPV to remove remaining vitreous or repositioning the tube into the anterior segment will be required.
Key Points
- The pars plana is an excellent location for tube insertion when the anterior chamber is not safe or available and may be the primary loca-tion whenever the eye has had a complete vitrectomy.
- Good communication and planning between surgeons is necessary to successfully combine glaucoma drainage device insertion and pars plana vitrectomy.
- Careful trimming of the vitreous skirt is important to prevent tube occlusion.
Suggested Readings
De Guzman MH, Valencia A, Farinelli AC. Pars plana insertion of glaucoma drainage devices for refractory glaucoma. Clin Experiment Ophthalmol. 2006;34(2):102-107.
Diaz-Llopis M, Salom D, García-Delpech S, Udaondo P, Millan JM, Arevalo JF. Efficacy and safety of the pars plana clip in Ahmed valve device inserted via the pars plana in patients with refractory glaucoma. Clin Ophthalmol. 2010;4:411-416.
Gandham SB, Costa VP, Katz LJ, et al. Aqueous tube-shunt implantation and pars plana vitrectomy in eyes with refractory glaucoma. Am J Ophthalmol. 1993;116(2):189-195.
Rothman RF, Sidoti PA, Gentile RC, et al. Glaucoma drainage tube kink after pars plana insertion. Am J Ophthalmol. 2001;132(3):413-414.
Smiddy WE, Rubsamen PE, Grajewski A. Vitrectomy for pars plana placement of a glaucoma seton. Ophthalmic Surg. 1994;25(8):532-535. </references>