Glaucomatocyclitic Crisis
| Primary authors |
|
|---|
Glaucomatocyclitic Crisis
Summary
•Described by Posner and Schlossman in 1948
•Acute, unilateral elevated IOP (70s) and low-grade anterior uveitis
•~50 years of age with unilateral blurred vision, corneal edema, pain and few small discrete round KP that resolve over weeks
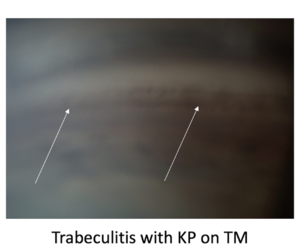
•Gonioscopy with KP over TM (trabeculitis)
•Chronic secondary glaucoma develops with repeated episodes
•Etiology unknown (? Herpes or autoimmune)
•Treat with IOP lowering medications and topical steroids with topical/oral NSAIDs.
•Chronic suppression with topical steroids or NSAIDs not helpful
•Prompt clinic visits are important to manage the disease
Video Lecture: https://youtu.be/9EnWVQyNyak
Introduction
Glaucomatocyclitic crisis, also known as Posner Schlossman Syndrome, is an acute, unilateral disease process with mild anterior chamber inflammation and elevation of intraocular pressure (IOP) that is recurrent. Damage to the optic nerve occurs after repeated attacks over a long period of time. The cause is unknown at this time despite several hypothesis which have been explored since the first cases were reported by Posner and Schlossman in 1948.
Clinical Presentation
The typical patient is 20-50 years old with complaints of mild ocular discomfort and blurring of vision. Examination reveals a mild inflammatory reaction in the anterior chamber with inferiorly distributed fine keratic precipitates (KP) and elevated IOP (up to 70 mmHg). Blurring of the vision and halos occur when corneal edema is present secondary to elevated IOP. The iris may become ischemic due to extreme IOP elevation and the pupil may be mid dilated. The conjunctival is often unremarkable. Gonioscopy reveals normal angle anatomy except for sparce inflammatory debris. KP are also identified over the trabecular meshwork (Figure 1) on gonioscopic examination. The patient may recall other similar episodes that are short lasting and may be separated by months or years, which adds to the diagnostic difficulty given the low likelihood of patients remembering episodes that occurred in the distant past. The optic nerve remains normal early in the course of the disease, but optic nerve cupping and visual field defects arise after multiple attacks. Examination of the anterior chamber and IOP between attacks are unremarkable often leading to confusion and delayed diagnosis.
Diagnosis
The diagnosis is often one of exclusion and as such, laboratory testing (viral PCR on aqueous humor) for HSV, VZV or CMV titers may be ordered to exclude infectious uveitis. Other possible etiologies that remain unproven include autonomic dysregulation, vascular endothelial pathology, allergic reactions, autoimmune disease or, as stated, viral infections.
Differential Diagnosis
Ocular Hypertension, Acute Angle Closure, Neovascular Glaucoma, Steroid Response Glaucoma, Uveitic Glaucoma (infections or Autoimmune), Fuchs’ Heterochromic Iridocyclitis should all be considered as part of the differential diagnosis. It is worth noting that Fuchs is also unilateral but rarely has IOP elevation to the degree seen with Glaucomatocyclitic Crisis, and the inflammation in Fuchs’ does not respond to anti-inflammatory therapy.
Treatment
IOP control is achieved with traditional topical pressure lowering drops. While some authors have advised avoiding prostaglandin analogues, there is no evidence that PGAs exacerbate the inflammation in this clinical scenario (or others for that matter). Pilocarpine should be avoided as it might lead to vascular leakage. Steroids have been used to treat inflammation although, as stated before, the attacks are short-lasting, and the inflammation frequently resolves without use of steroids. NSAIDs can also be used and may spare steroid related IOP spikes. Filtration surgery has been used in advanced disease to control spikes in IOP once glaucomatous optic neuropathy manifests.
Further Reading
1. Posner A, Schlossman A. "Syndrome of unilateral recurrent attacks of glaucoma with cyclitic symptoms." Arch Ophthalmol. 1948 Apr;39(4):517-35.
2. Hung PT, Chang JM. "Treatment of glaucomatocyclitic crises." Am J Ophthalmol. 1974;77:169–172.
3. Kass MA, Becker B, Kolker AE. "Glaucomatocyclitic crisis and primary open-angle glaucoma." Am J Ophthalmol. Apr 1973;75(4):668-73.