Postoperative Management of Glaucoma Drainage Implants
| Primary authors |
|
|---|
The postoperative management of glaucoma drainage implants is important in determining the success of the surgery. Patient education, medications, and in-office procedures are important things to consider when managing the postoperative glaucoma drainage implant patient.
Patient Education
The first part of successful glaucoma surgery is patient education. It is important to spend time educating your patients about what to expect, proper eye drop usage and compliance following surgery. Proper eye drop use is critical for postoperative intraocular pressure (IOP) control, inflammation treatment, and infection prophylaxis. Many glaucoma drainage implant patients may have medical conditions that make drop instillation difficult, such as dementia, arthritis, tremor, or coordination issues. In these patients, I find it helpful to elicit the aid of a reliable family member of the patient to assist with postoperative drop instillation. I like to provide a detailed sheet with drop instructions for the patient to take home following surgery. It is important to include bottle top colors and use large font to facilitate the reading and understanding of drop instructions. Giving patients a written schedule to follow, in a form they can understand and read, will improve compliance with complicated postoperative drop schedules.
As with any other intraocular surgery, it is important to tell patients to call if they notice worsening redness, pain, sudden loss of vision, discharge, or swelling. Most patients are very concerned about the appearance and comfort of their eye following tube shunt surgery. Foreign body sensation from sutures, moderate conjunctival injection, and subconjunctival hemorrhages are commonly seen following surgery. It is important to have patients look at their eye on the first postoperative day, so they know if the appearance of the eye changes for the worse. Educating patients on what to be concerned about and when to call their surgeon is an important first step in managing and avoiding problems following glaucoma drainage implant surgery.
Medications
A typical postoperative drop regimen for tube shunt surgery includes prednisolone acetate 1% 4 times a day and an antibiotic drop 4 times a day for the first week after surgery. If a patient is a known steroid responder, one can substitute loteprednol etabonate instead of prednisolone acetate. I prefer a flouroquinolone antibiotic for 1 week following surgery. I prefer a longer antibiotic course for some conditions, such as wound leaks, surface disease requiring contact lens use, or moderate to severe blepharitis. Higher doses of steroids may be necessary in patients with known uveitis or a predisposition to intraocular inflammation. Cycloplegics should be used when hypotony, shallow chamber, and choroidal effusions are present to facilitate anterior chamber deepening. Steroids and cycloplegics will help reduce the risk of peripheral anterior synechiae formation in the setting of hypotony.
Valved Implants
Typically, the steroids can be slowly tapered in the case of valved implants over the course of the first month or 2. They may need to be continued longer if a hypertensive phase develops. For further details on the hypertensive phase, please see this chapter.
When a valved glaucoma drainage implant is placed, flow is immediately established between the anterior chamber and the subconjunctival space over the implant, assuming that the valve is functioning and has been primed appropriately. This creates a higher likelihood of a low IOP in the immediate postoperative period for valved implants. These patients may need to be followed more closely during the early postoperative period for shallow chambers, hypotony, and choroidal effusions. Rarely, it may be necessary to reform the anterior chamber with viscoelastic if there is profound hypotony with a flat chamber in the early postoperative period (the reader is referred to the next section for further details on viscoelastic injections). In most cases, the early hypotony seen on valved implants can be managed with cycloplegics, steroids, and close monitoring. When hypotony is present, it is important to tell patients to avoid lifting, bending, or straining. I prefer to have them keep their head elevated on a pillow when sleeping and wear a protective shield at night. Typically, when there is hypotony following the implantation of a valved implant, it resolves in the first week or 2 with conservative treatment. Some surgeons advocate performing suture ligature of valved implants, such as the Ahmed, to avoid the risk of early postoperative hypotony.
Nonvalved Implants
Management Prior to Tube Opening
In a typical nonvalved implant, such as a Baervedlt or Molteno, there is a higher likelihood that you may be dealing with higher pressures in the immediate postoperative period due to the tube ligature and stent suture. These patients often need to restart their glaucoma drops and sometimes require oral carbonic anhydrase inhibitors following surgery until the tube opens. Initially, I like to start with aqueous suppressants. In general, I avoid prostaglandin analogues unless absolutely necessary out of concern for augmenting postoperative inflammation.
Because the nonvalved aqueous drainage implant is ligated in most cases in the early postoperative period, sometimes there is a need to lower IOP beyond what medicines can provide. In the very early postoperative period, one can use a TG -140 needle to fenestrate the tube proximal to the tube ligature site to allow egress of fluid through the fenestration. This can be done as a simple in-office procedure at the slit lamp. A betadine drop, antibiotic, and 2% lidocaine gel are placed in the eye. A temporal lid speculum is placed and a locking needle driver with a TG-140 needle is used to enter to subconjunctival space adjacent to the tube. The tube is then visualized anterior to the ligature suture and the needle is used to put a fenestration in the tube. The surgeon needs to take great care during this procedure to avoid violating the sclera and avoid globe perforation. The needle is then removed from the subconjunctival space after a fluid wave is observed. A cotton tip applicator is used to apply direct pressure to the needle entry site until no leak of aqueous is confirmed. This procedure can be accomplished when the ligature suture is visible posterior to the tissue patch graft. When placing the tube initially, I leave a little space between the tissue patch graft and the Vicryl ligature to allow for this type of in-office fenestration, if necessary. This technique can temporarily allow aqueous to be released until the tube opens.[1][2][3]
In addition to slit-lamp fenestrations, the tube can be opened early before the Vicryl suture dissolves. It is important to place the suture behind the tissue patch graft during the original surgery to allow access to the Vicryl ligature. Argon laser suture lysis of a Vicryl suture can be performed to open the tube prematurely using a 50-μm spot size, 500 mW, and 500 ms settings (Figure 12-1). I prefer not to open the tube prior to 4 weeks postoperatively to allow the capsule to mature and decrease the risk of hypotony. If forced to open the tube earlier in the setting of a very high pressure in a very advanced glaucoma patient, it is important to have viscoelastic (Healon or Healon GV, Abbott Medical Optics Inc, Abbott Park, Illinois) available to reform the anterior chamber if profound hypotony ensues.
If the surgeon uses a ripcord suture technique, pulling the ripcord can be a great way to increase the flow of aqueous to the bleb space over the implant if forced to do so by an unacceptable pressure. Again, it is better to wait as long as possible to pull the ripcord suture to allow adequate capsular maturation and lower the risk of hypotony. For very rare cases of unacceptable high IOP before the Vicryl dissolves, the ripcord suture can be removed. This can be done in the office by making a small incision in the conjunctiva overlying the suture with Vannas scissors, and gently removing the suture from the tube lumen with Jeweler’s forceps. It is especially useful for those eyes with orbital and lid anatomy that preclude visualization of the posterior tube, making laser suture lysis of the Vicryl ligature suture difficult. See this chapter for more details about the ripcord suture technique.
Management Following Tube Opening
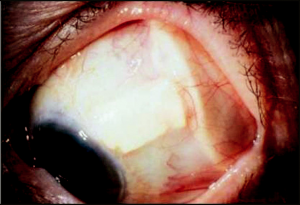
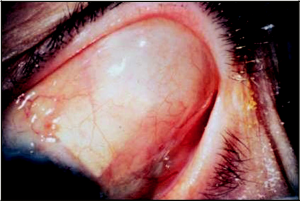
In tubes that are ligated, the type of suture used for ligature will determine when the tube will open. An 8 -0 Vicryl suture ligature typically opens at approximately 4 weeks and with a 7-0 Vicryl ligation suture it typically occurs 5 to 7 weeks postoperatively. When the tube opens, the ridge that is seen over the glaucoma drainage implant plate lessens, and a nice bleb is seen over the glaucoma drainage implant plate (Figures 12-2 and 12-3). It is important to see the patient more frequently around the time that the tube is likely to open. I often tell patients this is the second phase of the surgery and much akin to having a “second operation” in terms of frequency of follow-up. It is important to warn patients with ligated, nonvalved implants about the signs and symptoms of tube opening and need for immediate follow-up. Patients should call their surgeon if they notice a change in vision, increased redness, or pain. Some surgeons prefer to open the tube in the office at 5 to 6 weeks following tube placement, by lasering the Vicryl ligature or pulling the ripcord suture. It is often necessary to increase the frequency of steroid drops at the time of tube opening due to increased inflammation and sometimes fibrin formation. Some patients may exhibit profound inflammation following the tube opening with significant fibrin formation in the anterior chamber. In these cases, I have found it helpful to use 2 to 4 mg of subconjunctival dexamethasone, which can aid in controlling the inflammation. At times, a longer-acting steroid is needed and sub-Tenon’s triamcinolone acetate injection can be very effective.
Rarely, following tube opening, the presence of profound hypotony, with a flat chamber, may require injection of viscoelastic to maintain the chamber. I prefer to use regular Healon for the initial injection and move to a more viscous viscoelastic, such as Healon GV, if the patient fails initially with Healon. It is important to titrate the amount of viscoelastic used to reform the chamber to avoid a very high pressure. It is better, initially, to use only the amount necessary to deepen the chamber and assess for a response. A viscoelastic overfill can lead to very high pressures, which can require urgent viscoelastic removal. The injection of viscoelastic in the setting of profound hypotony and flat chamber will decrease the risk of a choroidal effusion or hemorrhage, chronic iridocorneal adhesions, or corneal decompensation. This technique should be used with caution in very advanced patients with visual field loss involving fixation, as there is a small risk of very high pressure following viscoelastic injections. It is important to warn patients to call immediately with increased eye pain or brow pain following a viscoelastic injection, which may indicate a high IOP. For management of patients in whom conservative measures fail to address the hypotony, the reader is referred to this chapter.
Key Points
- Valved implants tend to have lower IOP in the early postoperative period.
- Nonvalved implants, because of ligature and stent sutures, tend to have higher pressures in the immediate postoperative period. Patients and often need to be started back on glaucoma medicines until the tube opens.
- Fenestrations can provide immediate pressure lowering in a ligated, nonvalved glaucoma drainage implant until the tube has opened.
- Nonvalved implant patients need to be followed very closely around the time of tube opening because they can exhibit low IOP and increased inflammation.
- Treat inflammation aggressively to avoid inflammatory complications such as posterior or anterior synechiae, fibrin plug formation causing tube blockage, or pupillary membrane formation.
References
- ↑ Trible JR, Brown DB. Occlusive ligature and standardized fenestration of a Baerveldt tube with and without antimetabolites for early postoperative intraocular pressure control. Ophthalmology. 1998;105(12):2243-2250.
- ↑ Emerick GT, Gedde SJ, Budenz DL. Tube fenestrations in Baerveldt Glaucoma Implant surgery: 1-year results compared with standard implant surgery. J Glaucoma. 2002;11(4):340-346.
- ↑ Kansal S, Moster MR, Kim D, Schmidt CM Jr, Wilson RP, Katz LJ. Effectiveness of nonocclusive ligature and fenestration used in Baerveldt aqueous shunts for early post-operative intraocular pressure control. J Glaucoma. 2002;11(1):65-70.