Pseudoexfoliation
| Primary authors |
|
|---|
Pseudoexfoliation
1 Slide in 5 Minutes Video Lecture: https://youtu.be/Mu_EnYdIFUQ
Expanded Transcript:
The topic today is pseduoexfoliation. The fun starts right when you say the name because the name in itself is controversial. Some people advocate for calling it “exfoliation” while others have stuck with the term “pseduoexfoliation”. Pseudoexfoliation should not be confused with ”True Exfoliation” syndrome which is a rare disease classically linked to glassblowers (see the extended transcript for more details on this specific disease). The factors leading to pathology are thought to be linked to repeated exposure to heat and infrared radiation which causes lens capsule degeneration manifesting as dehiscence and schisis with delamination. I use the term pseudoexfoliation for the topic of focus today, as do the majority of people in the field, and so I will use that term here.
Pseudoexfoliation syndrome (sometimes abbreviated as PXF or PEX) is a systemic syndrome that is age-related (over age 50 with a much higher incidence in those over 70) and involves ocular tissues with the gradual deposition of fibrillary material on the lens capsule, zonules, trabecular meshwork, corneal endothelium, iris/pupillary margin and other tissues. The fibrillar material is thought to be due to abnormal turnover of the extracellular matrix in basement membranes. (elastic fibers, including fibrillin and α-elastin, and laminin, a component of basement membranes). The disease is typically bilateral and asymmetric with one eye sometimes not manifesting overt signs of disease until later in the follow up period. Some studies have shown associations with cardiovascular disease including myocardial infarction, stroke and high blood pressure. The iris also manifests vascular abnormalities in the form of hypoperfusion, microneovascularisation, and anastomotic vessels on iris fluorescein angiography. The “moth eaten” pupillary margin pattern of PXF is thought to be due to focal membrane disruption in melanin-containing epithelial cells. There is a genetic component linked to the LOXL1 gene which relates to enzymes that cross-link collagen and elastin in the extracellular matrix. One common misconception that comes up in teaching sessions is that PXF is exclusive to populations in or coming from northern Europe. We see PFX from all parts of the world with some African communities as well as native American communities showing high prevalence in multiple studies to date.
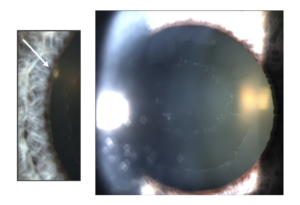
On examination, you can see all of the deposits mentioned above including fibrillar material on the lens capsule and drainage angle. The capsule manifestation is classically described as a bulls eye pattern which you can see in the photo (Figure 1). The bulls eye pattern is created by the iris chaffing away material in the deposit free zone each time the pupil dilates and constricts. Zonular laxity often results in phacodenesis. For the new residents out there, phacodenesis is when you see the lens move as the patient looks from side to side or if you bump the slit lamp and see the lens shake. The video shows a pseudoexfoliation cataract post femto rhexis and lens segmentation and the perilimbal heme from the femto suction docking system. The eye is exhibiting micromovements of the lens as the eye moves from side to side. The surgeon chose to use the femto laser in order to use as little pressure as possible in an eye with compromised zonules. This must be noted prior to cataract surgery so you can plan accordingly for a safe extraction of the lens as it is better to plan ahead for all the possibilities. More on this in a bit. The zonular laxity can also lead to shifting of the lens anteriorly with narrowing of the angle and potential angle closure. I’ve only seen this a handful of times in my career but it is more common in other areas where PXF is more prevalent.
The angle deposits are classically in clumps (compared to the even velvety appearance to pigment deposits seen in pigmentary glaucoma) with areas of more deposits in some areas compared to others. The deposits collect iris pigment cells and become pigmented over time. The angle also has the classic Sampaolesi line (which is pigment accumulation anterior to and on schwalbe’s line) also seen in pigment dispersion syndrome, a topic for a later date) and the obstruction in PXF is mainly mechanical with plugging of the outflow pathway and increase IOP which in some cases can be extreme. Approximately 40% of eyes with pseudoexfoliation develop glaucoma over time. The development of optic neuropathy may also relate to elastin dysfunction in the lamina cribrosa. We have already mentioned the moth-eaten pupillary margin that can be visible (see the picture) and the pupillary margin also frequently exhibits a buildup of PXF fibrilar material.
Performing cataract surgery can independently decrease the IOP in pseudoexfoliation patients, mainly due to washout of the deposited material, but the disease process persists, and cataract extraction is not curative. Some countries (Germany to name one) around the world that have “trabecular meshwork vacuum cleaners” that are used to wash out the PXF material at the time of cataract surgery and this can help decrease pressure but unfortunately is also short lasting as the fibrillar material builds up again over time. The “vaccum cleaner” efficacy highlights one difference between PXF and pigment dispersion. Pigment dispersion with accumulation in the angle can be toxic to the TM cells and the disease process is different from that caused by PXF deposits which mechanically plug the outflow pathway without the same toxicity seen from pigment cell accumulation. Simply washing out the pigment in pigment dispersion does not lower IOP.
When performing cataract surgery, the surgeon must be alert to the following possible complications:
• Shallow AC due to zonular instability should be expected and fluidics become extremely important in maintaining the AC depth and stability. • Poor pupillary dilation (due to degeneration of both sphincter and dilator muscles) often leads to use of iris expansion rings and iris hooks. Epi-Shugarcaine (or other variation) may also be used with proper surgical pre-planning to anticipate these issues. • Corneal Endothelial Health is compromised in PXF. Eyes with pseudoexfoliation syndrome and without glaucoma have lower endothelial cell count compared to control eyes and eyes with pseudoexfoliation glaucoma have significantly lower endothelial cell density compared to healthy eyes, eyes with pseudoexfoliation without glaucoma, and in normotensive fellow eyes. The exact reason for lower endothelial cell count is controversial and may in part be due to spikes in IOP but is likely multifactorial. • Phacodenesis has already been discussed and is hopefully noted preoperatively, but sometimes it becomes more obvious intraoperatively and the management skills above will help. • Zonular dialysis is more common with cataract surgery in PXF patients and can be managed with capsular hooks to assist in removal of any remaining lens fragments (or at start of surgery to maintain integrity of the bag post capsulorhexis when anticipated and sometimes foreshadowed by capsular wrinkling is noted during the rhexis creation) and CTRs can help maintain both intraoperative and postoperative capsular bag stability.
Cataract surgery in PXF patients is certainly a topic which is worth its own expanded deep dive and we can revisit in a future lecture.
Treatment:
• Medications: Typical classes work well and IOP control usually requires more than one medication. • Selective Laser Trabeculoplasty (SLT): Works very well but is shorter lasting due to plugging of the TM and can be repeated with caution. Lower energy should be used since the pigmented angle will result in more TM damage if higher energy is used. Some surgeons choose to treat 180 degrees at a time to avoid spikes. I treat 360 but keep the power setting to 0.4mJ. • MIGS: Pick your favorite. Bypassing the TM works well in PXF and most devices (implants or non-implants) will do well in PXG. • Trabeculectomy/Tubes: As per routine by the surgeon with close follow up for IOP spikes. • A note on cataract surgery: It is best not to wait long on PXF cataracts. These lenses should be removed at first sign of visual issues as it will only get harder to remove them later and cataract extraction has IOP lowering capacity that can help the patient as well.
In summary:
Pseudoexfoliation is a systemic disease with serious ocular manifestations related to the gradual deposition of fibrillary material on the lens and within the drainage angle leading to elevated IOP and glaucoma in 40% of cases. Patients are over 50 years of age and the disease manifestation is bilateral but often asymmetric. Young surgeons should be on the lookout for subtle findings on slit lamp exam including moth eaten pupillary margin and pigmented deposit clumps overlying the trabecular meshwork and sampaolesi line. Dilated examination will reveal deposits on the lens capsule and sometimes a bulls eyes configuration that is classic for PXF. Cataract surgery can be complicated and anticipating potential issues will give the best chance for a good outcome. Treatment involves the traditional med/laser, MIGS, Filtration surgery paradigm with the caveat that IOP lowering from standalone cataract surgery and laser trabeculoplasty often exhibit shorter lasting efficacy due to buildup of PXF deposits.