Selective Laser Trabeculoplasty
| Primary authors |
|
|---|
Video Lectures
SLT: Tips and Tricks: https://youtu.be/9T3qcd98x1k
LiGHT Trial Review: https://www.youtube.com/watch?v=_uz6wtm5fbM (see extended transcript below)
Introduction
Laser photocoagulation to the trabecular meshwork has been in use since the early 1970s.[1] First described by Worthen and Wickham in 1974, laser trabeculoplasty was initially performed using an argon laser.[2] It was not until 1979, when Wise and Witter[3] modified the argon laser trabeculoplasty (ALT) technique, that the procedure became widely accepted as a modality for the treatment of primary OAG and some forms of secondary OAG. The Glaucoma Laser Trial demonstrated that ALT is at least as effective as timolol in the treatment of OAG, and thus may be used as either a primary or adjunctive method to lower the intraocular pressure (IOP).[4] Numerous histologic studies have shown that coagulative damage occurs to the trabecular meshwork with ALT. It is believed that this struc-tural damage to the trabecular meshwork limits the success of retreatment with ALT.
Selective laser trabeculoplasty (SLT), based on the concept of selective photothermolysis, selectively targets pigmented trabecular meshwork cells while avoiding thermal and mechanical damage to neighboring cells.[5] Approved for use by the United States Food and Drug Administration in March 2001, SLT has gained acceptance among ophthalmologists as a safe and effective alternative to ALT for lowering IOP.
Background and Mechanism of Action
In 1983 Anderson and Parrish selectively targeted pigmented structures in vivo by manipulating optical radiation parameters.[5] In 1995 Latina and Park[6] conducted a study using various lasers to selectively target the pigmented trabecular meshwork cells while sparing the adjacent nonpigmented cells. These studies led to the development of the current 532-nm, frequen-cy-doubled, Q-switched Nd:YAG SLT laser.

The precise mechanisms of action of the ALT and SLT lasers remain poorly understood (Figure 1). However, 3 theories have been proposed to explain how these lasers lower IOP.
Mechanical Theory
Electromagnetic energy produced by the argon laser is transformed into thermal energy when it comes into contact with the trabecular meshwork. This thermal energy results in collagen shrinkage and tissue contraction, which leads to mechanical stretching of the surrounding uveoscleral tissue and widening of Schlemm’s canal. This structural change increases the passage of aqueous humor through the meshwork and into Schlemm’s canal, thus lowering the IOP.[7][8] Histological evidence exists to support this theory only for ALT.
Biologic Theory
Thermal energy generated by the laser stimulates increased cellular activity.[9] Studies involving both the ALT and SLT lasers have shown an upregulation of various cytokines, including interleukin (IL)-1 and tumor necrosis factor (TNF)-α, which leads to the recruitment of macro-phages into the trabecular meshwork and upregulation of matrix metalloproteinase expression with subsequent remodeling of the extracellular matrix and increased aqueous outflow.[10][11] Studies involving SLT have not shown scarring or contraction of the trabecular meshwork tissue (which is inconsistent with the mechanical theory) but rather favors the biologic theory.[12]
Repopulation Theory
One study specifically examining the ALT laser suggested the laser energy stimulates increased cell division and trabecular meshwork repopulation. These new cells were found to repopulate the burn sites where aqueous filtration occurs.[13]
Method of Treatment for Selective Laser Trabeculoplasty
As described above, the SLT is a 532-nm, frequency-doubled, Q-switched Nd:YAG laser. It has a 3-ns pulse duration and a spot size of 400 μm. Post-laser IOP spikes may possibly be reduced with pretreatment with a topical alpha-agonist (apraclonidine 0.5% or brimonidine tartrate 0.2%). After topical anesthesia is accomplished, either a Goldmann 3-mirror lens or Latina SLT lens (Ocular Instruments Inc, Bellevue, Washington) is used to focus the aiming beam onto the trabecular meshwork. The large spot size covers the entire width of the trabecular meshwork, making application of the laser beam easier. Studies have not conclusively demonstrated how much of the angle should be treated to achieve the maximum IOP lowering effect. However, ophthalmologists tend to apply either 50 nonoverlapping spots to 180 degrees (the superior, inferior, nasal, or temporal 180 degrees can be treated) of the angle or treat the full 360 degrees with 100 spots. The initial energy setting is 0.8 mJ per pulse, which is titrated to achieve the end point of visible “champagne bubbles” with 50% or more of the applications. In eyes with heavily pigmented meshwork, it is recommended to lower the initial setting (to 0.6 to 0.7 mJ) to prevent a postlaser IOP spike; the amount of angle treated or the number of laser spots may also be reduced in these eyes. After the procedure is completed, the same pretreatment glaucoma medications may be instilled into the eye. The IOP is typically checked 30 to 60 minutes after laser. A corticosteroid or nonsteroidal anti-inflammatory agent may be given to the patient to be used approximately 4 times a day for several days following SLT, depending on the treating physician’s preference. The prescribed glaucoma medications the patient was taking prior to the laser are typically continued until the efficacy of the laser is determined. The effect of the laser can be seen as early as the first week, but generally at least 4 to 6 weeks are allowed before determining the success of the laser.[14][15][16]
Indications and Contraindications for Selective Laser Trabeculoplasty
Indications[17]
- Primary open-angle glaucoma, exfoliation glaucoma, or pigmentary glaucoma.
- Glaucoma with medically uncontrolled IOP.
- Previously failed ALT.
- Patients with poor glaucoma medication compliance.
- Patients who cannot afford glaucoma medications.
- Patients who would like to reduce the number of glaucoma medications they are taking.
- Patients who do not tolerate glaucoma medications.
Contraindications[17]
- Inadequate visualization of the trabecular meshwork.
- Neovascular glaucoma.
- Active uveitis or history of uveitis (relative contraindication; see Further Study Needed section.
- Traumatic glaucoma (relative contraindication; see Further Study Needed section).
- Congenital or early childhood glaucoma (relative contraindication; see Further Study Needed section).
- Primary or secondary angle-closure glaucoma (relative contraindication; see Further Study Needed section).
Efficacy Rates
Selective Laser Trabeculoplasty Versus Argon Laser Trabeculoplasty
Several studies, both retrospective and prospective, have compared the IOP-lowering efficacy of ALT to SLT in open -angle glaucoma. In these studies, some eyes had been previously treated with ALT. Most of these initial studies involved a follow-up period of 6 to 12 months and demonstrated that both lasers produce a statistically equivalent IOP reduction at both 6 and 12 months postlaser.[14][17][18][19] Longer-term follow-up ranging to 60 months also describes similar rates of IOP reduction between the 2 laser types.[20]
Selective Laser Trabeculoplasty After Failed Argon Laser Trabeculoplasty
In one study, patients with prior failed ALT received treatment with 180 degrees of SLT and their IOP reduction was compared with patients who received SLT as an initial treatment.[17] No difference in IOP reduction was observed between the 2 groups. Another study found a greater IOP reduction (6.8 mm Hg) in a failed prior ALT group treated with SLT versus repeat ALT (3.6 mm Hg).[21] These studies suggest that SLT can effectively reduce the IOP even after failed ALT.
Selective Laser Trabeculoplasty Versus Glaucoma Medications
The SLT MED Study,[22] which is a prospective, randomized trial comparing SLT to topical medications as initial glaucoma therapy, showed after at least 8 months of follow-up that patients randomized to receive SLT achieved a mean IOP reduction of 6.7 mm Hg, whereas those in the medication group achieved a mean IOP reduction of 7.6 mm Hg. One study observed that after 12 months, SLT provided a mean IOP reduction of 31%, whereas topical latanoprost had a mean IOP reduction of 30.6%.[23] It has also been shown that 360 degrees of SLT provides an equivalent IOP reduction as latanoprost 0.005% once daily at night, whereas medication provides superior IOP lowering compared with 90- or 180-degree SLT treatments.[24]
Repeatability of Selective Laser Trabeculoplasty
It has been suggested that SLT can be repeated due to the apparent lack of structural damage to the trabecular meshwork from this laser. The repeatability of the SLT laser, in addition to its easier technical use, would give SLT some advantage compared with ALT. However, long-term prospective studies evaluating the repeatability of SLT have yet to be performed. One published study showed that SLT can lower IOP successfully in the short-term after prior SLT treatment.[25] Other results suggesting similar findings are as of yet unpublished.[26] Although these reports involve small patient populations, their results are encouraging and further exemplify the need for further studies in this area.
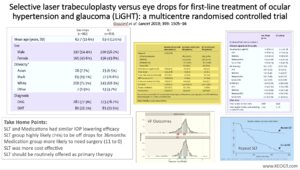
Primary Selective Laser Trabeculoplasty
The Laser in Glaucoma and Ocular Hypertension (LiGHT) Trial was a multicenter randomized controlled trial conducted to establish whether initial treatment with SLT was superior to initial medical therapy in treatment-naive patients with open angle glaucoma or ocular hypertension.[27] The parameters studied included health-related quality of life, cost-effectiveness, and clinical efficacy at 36 months. The study sites enrolled 718 patients, 356 were randomized to SLT and 362 to topical drops.[28] Quality of life questionnaire findings were similar between groups. At 36 months, 74·2% of patients in the SLT group did not require to maintain IOP at target. Eyes of patients in the SLT group were within target IOP at more 93·0% of visits compared to 91.3% for eyes on topical therapy. Glaucoma surgery was required for lowering of IOP in none of the SLT patients versus 11 patients in the medication group. There was a 97% probability of SLT as first treatment being more cost-effective than topical drops. The study authors concluded that SLT should be offered as a first-line treatment for open angle glaucoma and ocular hypertension.
A lecture on the LiGHT Study can be found here: https://www.youtube.com/watch?v=_uz6wtm5fbM
Extended Video Transcript
This is Malik Kahook from The University of Colorado and this is the second edition of one slide in 5 minutes. The topic today involves the elevation of primary Selective Laser Trabeculoplasty, or SLT, from a “side consideration” to a therapeutic approach that is much more common. The Laser in Glaucoma and ocular HyperTension Study, also known as the LiGHT Study (Figure 2), recruited consecutive, newly referred patients who were identified at six hospitals across the UK between 2012, and 2014. The study duration was 36 months.
Eligible patients had newly diagnosed, untreated open angle glaucoma (including a small number of pseudoexfoliation patients) or ocular hypertension in one or both eyes. Humphrey Visual Field (HVF) mean deviation requirement was no worse than –12 dB in the better eye or –15 dB in the worse eye and corresponding damage to the optic nerve. Patients were 18 years of age or older with visual acuity of 6/36 (20/120) or better in the eyes to be treated. Pervious ocular surgery was an exclusion, except uncomplicated phacoemulsification performed a year or more before randomization. Exclusion criteria also included contraindications to SLT (for example if the patients were unable to sit at the slit-lamp mounted laser, any past history of uveitis, or poor view of TM on gonioscopy), if they were unable to instill eye drops, had visually significant cataract, or those being treated for any ophthalmic condition.
It is important to note that clinicians and patients were not masked to the specific treatment arm. This was done in part to minimize the risk of the patient being less adherent to future drop use if they had received SLT initially and might believe they didn’t need to use drops. However, all measurements influencing treatment decisions (including visual field, optic disc imaging, and intraocular pressure measurements) were made by clinicians masked to treatment allocation. In cases where both eyes in the same patient were eligible, treatment was identical for both eyes. In both groups, patient mean age was ~62-63years, most patients were Caucasian (68-71%), most eyes where phakic and only a small subset of the OAG patient had Pseudoexfoliation --12 Meds (1.9%) 5 SLT (0.8%). Of note, pigmentary glaucoma patients were not included.
IOP goal was determined from both a percentage reduction (20% or 30% depending on disease status) from a single untreated baseline measurement (OHTS also used a single untreated baseline measurement but, unlike OHTS, the LiGHT study did not have any IOP eligibility criteria for enrollment, a strategy that can minimize Regression to the Mean).
Treatment escalation occurred if there was: (1) strong evidence of disease progression independent of intraocular pressure, (2) IOP above the target by more than 4 mm Hg at a single visit, or (3) IOP above the target by less than 4 mm Hg and less strong evidence of progression. Target IOP was decreased by 20% if disease progression was identified despite the measured IOP being at or below the set target level.
In the case of IOP above target by less than 4 mm Hg and no evidence of deterioration, the target IOP was revised to the mean of the previous three visits over which deterioration had not occurred. While this might seem a bit confusing… it is the way I practice in every day patient care. We are constantly revisiting our goal IOP based on specific clinical information as we engage with patients in clinic.
SLT treatment was completed over 360° of the trabecular meshwork using 100 non-overlapping shots (25 per quadrant), with the laser energy ranging between 0.3 to 1.4 mJ. Laser energy was to be titrated to observation cavitation bubbles and then the energy was decreased until bubbles were barely observable at least 50% of the time.
Re-treatment with SLT was allowed once if the initial treatment was noted to result in some lowering of IOP after the initial treatment. The next escalation was medical therapy for the SLT group. Repeat SLT was not done if the patient experienced complications from the initial treatment (ex. a spike in IOP). For the medical therapy arm, first line was prostaglandin analogues, second line was a blocker, third or fourth line was topical carbonic anhydrase inhibitors and alpha agonists. Systemic carbonic anhydrase inhibitors were only permitted while awaiting surgery. The study did not use SLT treatment for the drop arm prior to performing glaucoma surgery once maximum tolerated medical therapy was unsuccessful. Back to this point in a bit.
Data for the primary outcome were available for 652 (91%) of 718 patients at 36 months (92% of SLT group and 89% of the eye drops group) and were included in the intention-to-treat analysis.
Out of 718 patients, 517 (72.0%) were eligible in both eyes and 201 patients (28%) had only one eye eligible.
Overall 95% of eyes treated with SLT were at target IOP at 36 months. Target IOP was achieved without IOP medication in 78.2% of the eyes treated in the SLT group; of these 76.6% required only one treatment. A total of 74.2% of the patients in the SLT group were not using any drops at the 36-month visit. In comparison, 93.1% of the eyes treated in the eye drops group were at target IOP at 36 months, and 64.6% of patients were only using one medication.
Thirty-six eyes in the eye drops group had disease deterioration with three eyes converting from ocular hypertension to OAG and 33 eyes showing progression of OAG. In the SLT group, 23 eyes had disease deterioration with two eyes converting from ocular hypertension to OAG and 21 eyes showing progression of OAG. Cataract surgery was more common in the drop group (25) vs the drops group (13). The mean (SD) total power of initial SLT was 89.1mJ (+/-27.5) and the total number of applications was 98.9 (+/-4.6) shots.
Complications were minimal post SLT with one case of herpes simplex keratitis reactivation (also noted in one patient in the drops group) and two cases of uveitis (with one noted in the eye drops group). Only one eye required treatment due to IOP rise and resolved quickly with oral Acetazolamide.
One key finding was the requirement for glaucoma surgery (trabeculectomy) in 11 eyes (1.8%) in the eye drops group compared with none in the SLT group. Getting back to an earlier point, it is unclear how allowing SLT prior to surgery in the drops group might have influenced this, but my experience is that SLT does not perform as well in medicated eyes compared to treatment naïve eyes and the difference in surgery requirement remains significant in my mind despite this potential confounding issue.
Some other findings, from a cost perspective, SLT was found to be more cost effective than the drops first approach and took into consideration the cost of procedures, medications, follow-up visits and other parameters (non-eye related costs) that influence quality of life. There were more follow up visits in the SLT arm but there were more follow-up visits mandates in this group to be seen earlier post laser treatment.
There was a lack of quality of life differences between group which might be attributed to the type of questionnaire used with the focus more on the disease effect rather than the treatment effect and could be an area of further exploration in the future.
The authors concluded that primary SLT is a cost-effective alternative to drops that can be offered to patients with OAG or ocular hypertension needing treatment to lower IOP with the caveat that communication with the patient is key due to the possibility of some patients believing close monitoring is not necessary after laser (essentially fear that post laser patients might believe they are cured). My feeling is that adherence to follow up visits is poor across the board and not unique to patients post SLT compared to those receiving drops.
Two follow up LiGHT study publications are worth brief mention:
A study by Wright and colleagues looked at differences in VF progression (9 VFs over 48 months) between the two groups in the LiGHT study and found, using total deviation values, that 1 in 4 eyes in the medication group showed moderate or fast VF progression, whereas in the SLT group, this value was approximately 1 in 6. The authors concluded “With slower VF deterioration, SLT may delay or completely avert the need for more intense medical and surgical intervention in a significant proportion of patients.”
The second study by Garg and colleagues set to determine the efficacy of repeat SLT in the LiGHT study in patients requiring repeat treatment for early to medium-term failure of initial SLT treatment. 115 eyes of 90 patients received repeat SLT during the first 18 months of the study. Kaplan-Meier analysis of initial SLT survival demonstrated a median duration of effect of 189 days. Median duration of survival post repeat SLT could not be determined because 50% of these eyes did not reach the end point within the 18-month follow-up period, although available data show that median duration of survival in this group was at least 18 months. The Pre-treatment IOP before initial SLT was significantly higher than that before repeat SLT. A total of 34 eyes were early failures (retreated at 2 months after initial SLT) and 81 were considered late failures (retreatment after 2 months from initial SLT). The authors concluded that repeat SLT maintained drop-free IOP control in 67% of 115 eyes at 18 months. This is strong evidence that repeat SLT should be considered much earlier than would I would have considered in the past and that outcomes post repeat SLT can be clinically meaningful as well as long lasting and may obviate the need for adding drops or needing surgery to lower IOP for an extended period of time.
I was able to join Gus Gazzard and a few other colleagues on webinar where we discussed the LiGHT trial findings and Dr. Gazzard summarized the take home points as follows:
· Laser 1st gave drop-free disease control in 74% of patients at 3 years with less surgery and lower cost
· SLT was safe
· Primary SLT was associated with less rapid progression of visual field loss
· Repeat SLT was at least as effective as initial SLT treatment
My personal conclusion is that I should be offering more primary SLT to treatment naïve patients compared to what I have done in the past and I would welcome future exploration of adding SLT vs medications in patients already on one or two drops when treatment escalation is needed.
Selective Laser Trabeculoplasty’s Effect in Specific Patient Subgroups
Type of Glaucoma
- Exfoliation glaucoma: Just as ALT has been shown to be at least as effective in exfoliation glaucoma as in primary open-angle glaucoma eyes, studies comparing SLT in these 2 groups of patients show similar findings with comparable success rates. There is some minor evidence that the effects of SLT in exfoliation glaucoma patients may last somewhat longer than in primary open-angle glaucoma patients.[16][29]
- Pigmentary glaucoma: For SLT in pigmentary glaucoma, please see the following section.
Degree of Trabecular Meshwork Pigmentation
Most studies have not found a relationship between the degree of trabecular meshwork pigmentation and the success rates of SLT. These studies have included a small number of pigmentary glaucoma patients who have had similar SLT success rates when compared with patients with less trabecular meshwork pigment.[16][29]
The literature does contain case series of pigmentary glaucoma patients who have experienced sustained post-SLT IOP spikes, however. Some of these patients required trabeculectomy shortly after SLT to control the IOP.
The authors of these series suggest that the SLT parameters be altered for pigmentary glaucoma patients. For instance, lower energy levels, fewer laser spots, or treating a smaller circumference of the angle at each session should be considered. The treating ophthalmologist should monitor the post-SLT IOP especially carefully in these patients.[30]
Level of Preoperative Intraocular Pressure
Several studies suggest that SLT tends to be more successful in eyes with higher preoperative laser IOPs, at least when SLT success is measured as a percentage of IOP lowering from baseline.[31][32] This finding is similar to the published evidence that glaucoma medications also tend to reduce IOP more significantly in eyes with higher pretreatment pressures. One published study involving normal tension glaucoma patients who underwent SLT suggests that SLT does lower IOP in these patients to some degree and may also help reduce the amount of IOP fluctuation in this disease.[33]
Race
A paucity of studies exists regarding race in relation to SLT success, but one article did find that SLT and ALT had similar success rates in black and white patients.[20] Some studies performed in Asian populations showed that SLT had good success rates in these groups.[34][35]
Lens Status
Phakic and pseudophakic eyes seem to have similar responses to SLT, in terms of amount of IOP lowering and success rates.[36]
Prior Trabeculoplasty Treatment
- ALT: As described above, studies have shown that the efficacy of ALT and SLT are similar when comparing results up to 60 months after laser treatment.[16][20] There is no clear evidence that eyes with previous ALT have more adverse effects from SLT when compared with laser-naïve eyes undergoing SLT.
- SLT: The issue of SLT’s efficacy when repeated needs further study. One published article reports that repeat 360-degree SLT lowers pressure equally well to the first SLT treatment when performed at least 6 months after the original treatment has failed.[37]
Other Patient Subgroups
- Several studies in the literature have shown that SLT can be a useful adjunctive treatment in eyes that experience an IOP elevation after intravitreal triamcinolone injection. These eyes tend to also require topical glaucoma medications to control the IOP.[16][38][39]
- One study of SLT in diabetic versus nondiabetic eyes showed similar levels of efficacy.[40]
- One study described IOP lowering after SLT in eyes with chronic primary angle closure that had already been treated with laser iridotomy. In these eyes, SLT was applied to the portions of the trabecular mesh-work that were visible on gonioscopy.[41]
Adverse Effects of Selective Laser Trabeculoplasty
Fortunately, the vast majority of reported adverse reactions to SLT have been transient and without lasting sequelae. The most common reactions are described below.
Early Postoperative Intraocular Pressure Elevation
The most commonly reported adverse reaction after SLT is an early postlaser IOP elevation. Most studies report a significant pressure elevation as >5 mm Hg compared with pre-SLT levels. The occurrence rate of this pressure elevation ranged from 0% to 30%, depending on the study. Some study patients received a prophylactic pressure-lowering eye drop perioperatively (usually apraclonidine 0.5% or brimonidine tartrate 0.2%), whereas others did not. In several studies,[18][21][32] use of a prophylactic pressure-lowering eyedrop did not seem to affect the rate of postlaser pressure elevation. The majority of patients with a significant pressure elevation post-SLT respond well to additional topical medications and/or watchful waiting, with resolution of the pressure elevation. The exception to this was 3 reported patients with heavily pigmented trabecular mesh-work who had severe, prolonged IOP elevation after SLT and underwent trabeculectomy.[16][29][30]
Anterior Chamber Reaction
Although numerous studies report no anterior chamber reaction after SLT, some studies have described mild to moderate level of cells and flare. In all published studies, the anterior chamber inflammation was self-limited and resolved without long-term sequelae. No peripheral anterior synechiae were reported after these episodes of anterior chamber reaction.[16]
Pain
A few studies have noted small numbers of patients who experienced pain with SLT treatment.[18][24][42] There is a suggestion that of patients who felt pain with SLT, the pain level was significantly lower when compared with patients undergoing ALT.[42] One study described more patients experiencing pain during SLT when a larger circumference of the angle was treated compared to a smaller treatment area.[24]
Other Adverse Reactions
Other adverse reactions from SLT are rare. One case report is in the literature of self-limited hyphema occurring during SLT; this resolved spontaneously.[43] Four case reports were published indicating corneal edema, haze, and thinning. The corneal thinning persisted long-term in these cases.[44]
Further Study Needed
More work needs to done regarding the long-term effect of SLT, as well as its repeatability. Given the fact that SLT has few adverse effects, and if it is shown over time to be successful with repeated treatments, it may help influence the glaucoma treatment paradigm in our aging patient population. Regarding aging, investigating the efficacy of SLT in patients of different ages would be helpful. Studies addressing the interaction and possible synergy of SLT with medical glaucoma therapy also need to be performed. With more recognition and emphasis placed on the diurnal nature of IOP fluctuation, SLT’s effect on possibly blunting the pressure curve should be investigated.
Establishing optimal treatment parameters for SLT would help the thousands of ophthalmologists who currently perform this treatment. Currently, there is some disagreement on whether each laser session should involve treatment of 90, 180 or 360 degrees of the angle although more recent practice patterns have gravitated towards treating 360 degrees. Also, the effect of the number of applications and pulse duration has not been well studied. Post-laser anti-inflammatory treatment varies widely across practitioners, and although it had been suggested in the literature that using topical steroids short-term after SLT did not affect its success, the efficacy or necessity of this is not entirely agreed upon.[45] The SALT Trial examined whether short-term use of topical nonsteroidal anti-inflammatory drugs (NSAIDs) or steroid therapy affected the efficacy of SLT[46]. The trial concluded that eyes treated with steroid or NSAID drops after SLT had significantly better IOP reduction at 12 weeks compared to placebo treatment.
SLT has not been well studied in eyes in which ALT has not been considered useful. For instance, it is not known whether SLT is safe and effective in eyes with uveitic, angle recession, or congenital glaucoma. More studies addressing the efficacy of SLT in normal tension glaucoma, particularly with regard to diurnal fluctuation, are also needed.
Conclusion
SLT is a procedure that is gaining increasingly wider popularity due to its efficacy, favorable side- effect profile, technical ease, and potential repeatability. Ophthalmologists can consider SLT as primary or adjunctive treatment for elevated IOP. The evidence is clear that lowering IOP can effectively slow glaucoma disease progression and vision loss, and thus SLT is a useful tool in the armamentarium against this widespread disease. Further studies will clarify its role in terms of longer-term follow-up, repeatability, and usefulness in secondary glaucomas.
Key Points
- SLT can be useful as primary or adjunctive therapy for elevated IOP.
- SLT is relatively straightforward to perform and may yield benefits even when performed more than once.
- Side effects from performing SLT tend to be mild and self-limited; however, transient pressure spikes shortly after SLT have been reported, especially in eyes with heavy trabecular meshwork pigment.
- More research is needed to determine SLT’s usefulness in long-term follow-up, in certain secondary glaucoma populations, and in terms of repeatability.
References
- ↑ Van der Zypen E, Frankhauser F. Lasers in the treatment of chronic simple glaucoma. Trans Ophthalmol Soc UK. 1982 Apr;102(1):147-153.
- ↑ Worthen DM, Wickham MG. Argon laser trabeculotomy. Trans Am Acad Ophthalmol Otolaryngol. 1974;78(2):OP371-OP375.
- ↑ Wise JB, Witter SL. Argon laser therapy for open-angle glaucoma: a pilot study. Arch Ophthalmol. 1979;97(2):319-322.
- ↑ The Glaucoma Laser Trial Research Group. The Glaucoma Laser Trial (GLT). 2. Results of argon laser trabeculoplasty versus topical medications. Ophthalmology. 1990;97(11):1403-1413.
- ↑ 5.0 5.1 Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220(4596):524-527.
- ↑ Latina MA, Park C. Selective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactions. Exp Eye Res. 1995;60(4):359-372.
- ↑ Melamed S. Argon laser trabeculoplasty: how does it work? In: Epstein DL, Alling-ham RR, Schuman JS, eds. Chandler and Grant’s Glaucoma. 4th ed. Baltimore, MD: Lippincott Williams & Wilkins; 1997:466-469.
- ↑ Melamed S, Pei J, Epstein DL. Delayed response to argon laser trabeculoplasty in monkeys: morphological and morphometric analysis. Arch Ophthalmol. 1986;104(7): 1078-1083.
- ↑ Stein JD, Challa P. Mechanisms of action and efficacy of argon laser trabeculoplasty and selective laser trabeculoplasty. Curr Opin Ophthalmol. 2007;18(2):140-145.
- ↑ Melamed S, Pei J, Epstein DL. Short-term effect of argon laser trabeculoplasty: studies of mechanism of action. Arch Ophthalmol. 1985;103(10):1546-1552.
- ↑ Ruddat MS, Alexander JR, Samples JR, et al. Early changes in trabecular metallopro-teinase mRNA levels in response to laser trabeculoplasty are induced by media bome factors. Invest Ophthalmol Vis Sci. 1989;30(Suppl):280.
- ↑ Kramer TR, Noecker RJ. Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmol-ogy. 2001;108(4):773-779.
- ↑ Bylsma SS, Samples JR, Acott TS, Van Buskirk EM. Trabecular cell division after argon laser trabeculoplasty. Arch Ophthalmol. 1988;106(4):544-547.
- ↑ 14.0 14.1 Latina MA, de Leon JMS. Selective laser trabeculoplasty. Ophthalmol Clin N Am. 2005;18(3):409-419.
- ↑ Zao JC, Grosskreutz CL, Pasquale LR. Argon versus selective laser trabeculoplasty in the treatment of open angle glaucoma. Int Ophthalmol Clin. 2005;45(4):97-106.
- ↑ 16.0 16.1 16.2 16.3 16.4 16.5 16.6 Barkana Y, Belkin M. Selective laser trabeculoplasty. Surv Ophthalmol. 2007;52(6): 634-654.
- ↑ 17.0 17.1 17.2 17.3 Damiji K. Selective laser trabeculoplasty: a better alternative. Surv Ophthalmol. 2008;53(6):646-651.
- ↑ 18.0 18.1 18.2 Latina MA, Sibayan SA, Shin DH, et al. Q-switched 532 nm Nd:YAG laser trabeculoplasty (selective laser trabeculoplasty): a multicenter pilot, clinical study. Ophthalmology. 1998;105(11):2082-2088.
- ↑ Pirnazar JR, Kolker A, Way M, et al. The efficacy of 532 nm laser trabeculoplasty. Invest Ophthalmol Vis Sci. 1998;39(4):S5.
- ↑ 20.0 20.1 20.2 Juzych MS, Chopra V, Banitt MR, et al. Comparision of long-term outcomes of selec-tive laser trabeculoplasty versus argon laser trabeculoplasty in open-angle glaucoma. Ophthalmology. 2004;111(10):1853-1859.
- ↑ 21.0 21.1 Damji KF, Shah KC, Rock WJ, et al. Selective laser trabeculoplasty versus argon laser trabeculoplasty: a prospective randomized clinical trial. Br J Ophthalmol. 1999;83(6):718-722.
- ↑ Katz LJ, Steinmann WC, Marcellino GR; The SLT MED Study Group. Comparison of selective laser trabeculoplasty vs. medical therapy from intial therpay for glaucoma or ocular hypertension. Presented at: American Academy of Ophthalmology Annual Meet-ing; November 2006; Las Vegas, NV. Presentation #PO108.
- ↑ McIlraith I, Strasfeld M, Colev G, Hutnik CM. Selective laser trabeculoplasty as initial and adjunctive treatment for open-angle glaucoma. J Glaucoma. 2006;15(2):124-130.
- ↑ 24.0 24.1 24.2 Nagar M, Ogunyomade A, O’Brart DP, et al. A randomized, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br J Ophthalmol. 2005;89(11):1413-1417.
- ↑ Lai J, Bournias TE. Repeatability of selective laser trabeculoplasty (SLT). Invest Ophthalmol Vis Sci. 2005;46:E-Abstract 119.
- ↑ Nagar M. SLT—effect of enhancement and repeatability on IOP. Unpublished American Academy of Ophthalmology 2006 poster presentation.
- ↑ Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Laser in Glaucoma and Ocular Hypertension (LiGHT) trial. A multicenter, randomised controlled trial: design and methodology. Br J Ophthalmol. 2018 May;102(5):593-598.
- ↑ Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicenter randomised controlled trial. Lancet. 2019 Apr 13;393(10180):1505-1516.
- ↑ 29.0 29.1 29.2 Realini T. Selective laser trabeculoplasty: a review. J Glaucoma. 2008 Sep;17(6):497-502.
- ↑ 30.0 30.1 Harasymowycz PJ, Papamatheakis DG, Latina M, et al. Selective laser trabeculoplasty (SLT) complicated by intraocular pressure elevation in eyes with heavily pigmented trabecular meshworks. Am J Ophthalmol. 2005;139(6):1110-1113.
- ↑ Hodge WG, Damji KF, Rock W, et al. Baseline IOP predicts selective laser trabeculoplasty success at 1 year post-treatment: results from a randomized clinical trial. Br J Ophthalmol. 2005;89(9):1157-1160.
- ↑ 32.0 32.1 Song J, Lee PP, Epstein DL, et al. High failure rate associated with 180 degrees selective laser trabeculoplasty. J Glaucoma. 2005;14(5):400-408.
- ↑ El Mallah MK, Walsh MM, Stinnett SS, Asrani SG. Selective laser trabeculoplasty reduces mean IOP and IOP variation in normal tension glaucoma patients. Clin Ophthalmol. 2010;4:889-893.
- ↑ Lai JS, Chua JK, Tham CC, Lam DS. Five-year follow up of selective laser trabeculoplasty in Chinese eyes. Clin Experiment Ophthalmol. 2004;32(4):368-372.
- ↑ Shibata M, Sugiyama T, Ishida O, et al. Clinical results of selective laser trabeculoplasty in open-angle glaucoma in Japanese eyes: comparison of 180 degree with 360 degree SLT. J Glaucoma. 2010;21(1):17-21.
- ↑ Werner M, Smith WM, Doyle JW. Selective laser trabeculoplasty in phakic and pseudophakic eyes. Ophthalmic Surg Lasers Imaging. 2007;38(3):182-188.
- ↑ Hong BK, Winer JC, Martone JF, Wand M, Altman B, Shields B. Repeat selective laser trabeculoplasty. J Glaucoma. 2009;18(3):180-183.
- ↑ Pizzimenti JJ, Nickerson MM, Pizzimenti CE, et al. Selective laser trabeculoplasty for intraocular pressure elevation after intravitreal triamcinolone acetonide injection. Optom Vis Sci. 2006;83(7):421-425.
- ↑ Rubin B, Taglienti A, Rothman RF, Marcus CH, Serle JB. The effect of selective laser trabeculoplasty on intraocular pressure in patients with intravitreal steroid-induced elevated intraocular pressure. J Glaucoma. 2008;17(4):287-292.
- ↑ Leung EH. Modulation of SLT response in patients with diabetes—six month follow-up of the University of Chicago SLT study. Paper presented at: Annual Meeting of the Association for Research in Vision and Ophthalmology; May 2005; Fort Lauderdale, FL.
- ↑ Ho CL, Lai JS, Aquino MV, et al. Selective laser trabeculoplasty for primary angle clo-sure with persistently elevated IOP after iridotomy. J Glaucoma. 2009;18(7):563-566.
- ↑ 42.0 42.1 Martinez-de-la-Casa JM, Garcia-Feijoo J, Castillo A, et al. Selective vs argon laser trabeculoplasty: hypotensive efficacy, anterior chamber inflammation, and postoperative pain. Eye. 2004;18(5):498-502.
- ↑ Rhee DJ, Krad O, Pasquale LR. Hyphema following selective laser trabeculoplasty. Oph-thalmic Surg Lasers Imaging. 2009;40(5):493-494.
- ↑ Regina M, Bunya RM, Orlin SE, Ansari H. Corneal edema and haze after selective laser trabeculoplasty. J Glaucoma. 2011;20(5):327-329.
- ↑ Realini T, Hettlinger CJ. The impact of anti-inflammatory therapy on IOP reduction following selective laser trabeculoplasty. Ophthalmic Surg Lasers Imaging. 2010;41(1): 100-103.
- ↑ Groth SL, Albeiruti E, Nunez M, et al. SALT Trial: Steroids after Laser Trabeculoplasty: Impact of Short-Term Anti-Inflammatory Treatment on Selective Laser Trabeculoplasty Effiacy. Ophthalmology, 2019 Nov;126(11):1511-1516.
